Pancreatitis in dogs—which means inflammation of the pancreas—is a serious and even life-threatening medical condition. Integrative veterinarian Dr. Julie Buzby explains the signs, causes, and treatment options so you can help your dog have the best possible outcome if he or she is ever diagnosed with pancreatitis.

I rarely hospitalized patients when I owned my own veterinary hospital. My guiding principle was that pets were often better off overnight at home with their families than they were in my hospital alone. But I made an exception for a condition called pancreatitis. In fact, pancreatitis was one of the most common reasons that I hospitalized dogs and cats—including my sweet doggy patient Ellie.
This 10-year-old female Miniature Schnauzer sat looking miserable on my exam table. Her mom was rightly worried about her dear dog’s symptoms—loss of appetite, vomiting, lethargy, and a painful belly. I was glad that Ellie’s mom brought her dog to our hospital right away because I was worried she might have pancreatitis.
What is pancreatitis in dogs?
Pancreatitis is an inflammation of the pancreas. In dogs, pancreatitis tends to cause GI symptoms such as vomiting, diarrhea, and abdominal pain, and is most commonly associated with eating a high-fat meal. Unfortunately, pancreatitis can potentially be serious or even life-threatening. To understand what makes pancreatitis so problematic, you need to know a little about the pancreas.
The role of the pancreas
The pancreas is a critically important organ in your dog’s body that has two major functions, which veterinarians label as “endocrine” and “exocrine.”
The endocrine portion of the pancreas produces hormones (insulin and glucagon) and secretes them into the blood to control blood sugar. If the pancreas doesn’t make enough insulin, the end result is diabetes mellitus.
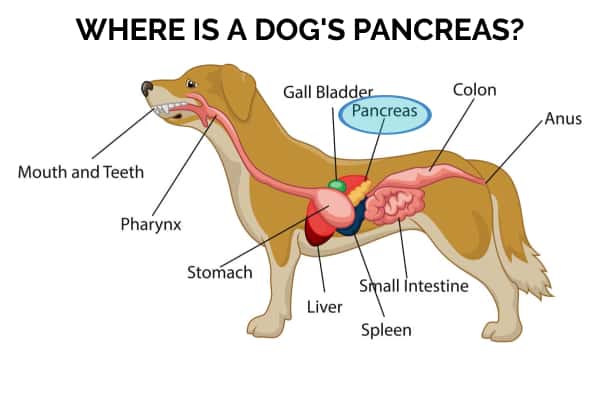
Additionally, the pancreas has a vital “exocrine” role, which is directly related to its position adjacent to the first part of the small intestines and close to the stomach and liver. It releases important digestive enzymes into the duodenum (the beginning portion of the small intestines) in a non-active form when your dog eats a meal. Then the digestive enzymes become activated in the small intestines and start to digest food.
In the case of pancreatitis, the digestive enzymes become activated inside of the pancreas instead of inside the small intestines. In a nutshell, the pancreas begins to digest itself. As you can imagine this is terribly serious and painful. On top of that, the damaged pancreas also leaks the activated enzymes into the abdominal cavity. This causes serious injury to other internal organs such as the liver and kidneys.
What are the symptoms of pancreatitis in dogs?
Signs of pancreatitis can vary. Some dogs display absolutely no signs, some have mild signs, and some have severe signs.

Common symptoms of pancreatitis in dogs
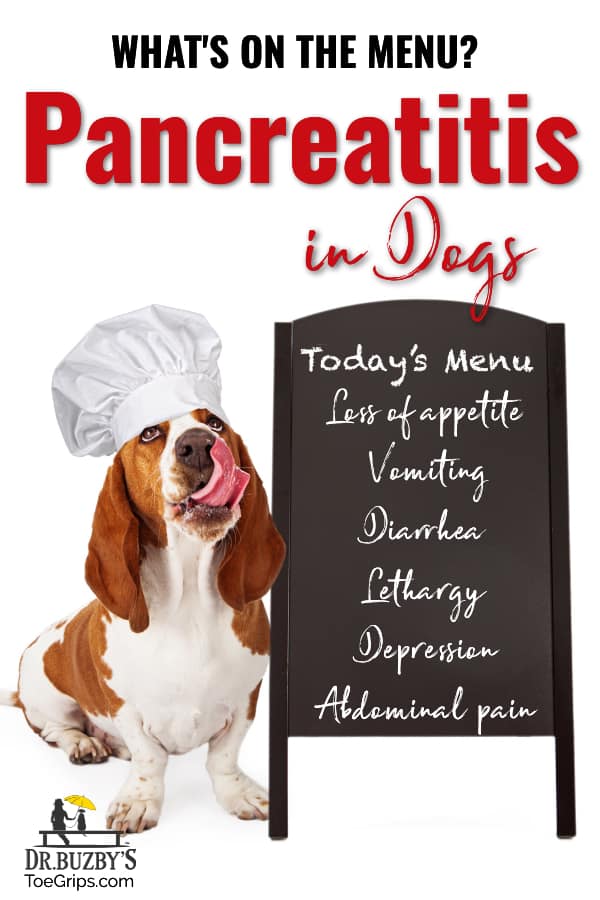
The most common signs of pancreatitis in dogs include:
- Loss of appetite—Dogs may have no interest in food, may only eat a small amount, or may just eat treats.
- Vomiting—In one study, approximately 90% of dogs with pancreatitis were vomiting. Sometimes the vomit may have blood in it (hematemesis).
- A lethargic dog—Your dog may be lying around more or acting tired
- Depression—Dogs with pancreatitis may have minimal interest in daily activities (walks, play time, petting, etc.)
- Diarrhea—The dog may have loose or watery stool or dog diarrhea with blood that is bright red (hematochezia)
- Abdominal pain—Dogs with abdominal pain may act tense or painful when you put pressure on the abdomen to pick them up. Or they may stand in a hunched “prayer” or “play bow” position and have a tense look on their face. Abdominal pain was present in 58% of dogs with pancreatitis in one study.
- Nausea—If the dog keeps licking his or her lips or drooling, he or she might be nauseous.

Signs that pancreatitis is getting worse
Additionally, it is important to be on the lookout for signs of worsening pancreatitis or severe pancreatitis, including:
- Collapse—Dogs with severe pancreatitis may become weak and be unable to stand or walk.
- Dehydration—Due to fluid loss from vomiting and/or diarrhea, the dog may exhibit signs of dehydration such as dry or sticky gums, sunken eyes, or skin that remains tented when lifted.
- Fever—Sometimes more severe cases of pancreatitis may cause a fever. It helps to know how to take your dog’s temperature so you can determine if your dog has a fever.
- Weakness—Trembling legs, moving slowly, or struggling to rise can all indicate that your dog is getting weaker.
- Dull or obtunded mentation—Your dog may seem to be processing things slowly or not be fully aware of what is going on around him or her.
- Shock—Elevated heart rate, pale gums, weakness, hypothermia (low body temperature), weak pulses, and collapse can all point to shock. This can be life-threatening
- Bruising—If the dog is having clotting issues (disseminated intravascular coagulation or DIC) due to severe pancreatitis, he or she may have petechiae (pinpoint bruises) or ecchymoses (larger bruises) on the skin or gums. This is also an emergency.
- Minimal or no urine production—In the case of kidney failure in dogs secondary to pancreatitis, the dog may not be making much urine.
If your dog might have pancreatitis, head to the vet without delay
If your dog’s symptoms are mild, you should make an appointment with your veterinarian. However, if your dog is experiencing severe symptoms, you may need to make an emergency vet visit instead. Pancreatitis is a serious, and sometimes deadly, condition so it is important to get help for your dog promptly.
What is the difference between acute and chronic pancreatitis in dogs?
It’s worth noting at this point that there are two categories or forms of canine pancreatitis—acute and chronic.
Acute pancreatitis in dogs
Acute pancreatitis, as the term “acute” would imply, has a sudden onset. Your dog is fine and then he or she is sick. Sometimes acute pancreatitis is mild, meaning that the dog shows minimal symptoms or perhaps slight GI upset or abdominal pain that resolves easily with treatment.
In other cases, acute pancreatitis can be severe. These dogs are very sick. They may have severe vomiting and abdominal pain, significant lethargy or weakness, and sometimes have free fluid in their abdomen.
Some dogs with acute severe pancreatitis do respond well to aggressive treatment. Unfortunately, other dogs will go into shock, multi-organ failure, or disseminated intravascular coagulation (a dangerous condition where the blood clots abnormally). These conditions may be fatal.
Recurrent acute pancreatitis
Some dogs are also prone to recurrent acute pancreatitis. This means their bout of pancreatitis resolves, but then they get acute pancreatitis again, possibly because of one of the triggers we will discuss soon.
Thus, once your dog has had pancreatitis, it is critical to try to decrease his or her risk factors. Some factors, such as breed or underlying medical conditions, can’t be changed. However, you do have control over your dog’s diet and weight.
Chronic pancreatitis in dogs
With chronic pancreatitis, symptoms will look the same as acute pancreatitis but tend to be milder as a general rule. Sometimes the exact cause of chronic pancreatitis is unknown. In other cases, it may happen due to recurrent bouts of acute pancreatitis or as a result of an autoimmune disorder found in English Cocker Spaniels.
However it develops, the symptoms of chronic pancreatitis tend to come and go due to long-term, smoldering inflammation of the pancreas. This leads to irreversible damage which may decrease the amount of functional tissue left in the pancreas.

Remember how we talked about what the pancreas does? Well, when enough tissue is destroyed, the pancreas can’t do its job anymore. This means the dog could develop diabetes mellitus due to a lack of insulin production. Or he or she could end up with exocrine pancreas insufficiency (EPI in dogs), a lack of digestive enzymes which causes poor absorption of nutrients from food.
With veterinary treatment, dogs may recover from bouts of chronic pancreatitis. However, they are more prone to future attacks of pancreatitis, which makes it all the more important to avoid possible triggers.
Causes of pancreatitis in dogs
Many pancreatitis cases are idiopathic, which means that there is no identifiable cause. However, there are some known risk factors. Check this list to see if your dog is at higher risk for pancreatitis.

1. Certain breeds may be predisposed to pancreatitis.
Yorkshire Terriers, Dachshunds, Poodles, Cavalier King Charles Spaniels, Terriers, and Cocker Spaniels all have a genetic predisposition toward pancreatitis. This puts them at a higher risk than dogs of other breeds. However, keep in mind that any breed of dog can get pancreatitis.
Miniature Schnauzers, like my patient, are the most common breed identified in studies on pancreatitis. This may have something to do with the fact that Schnauzers are more likely to have higher fat content in their blood than other dog breeds. This condition, known as hyperlipidemia (hyper = high, lipid = fat, -emia = in blood), increases the risk of pancreatitis.
2. A high fat meal may be the culprit.
When your dog eats food that isn’t a normal part of his or her diet, he or she is at a higher risk for gastrointestinal upset like vomiting and diarrhea. New foods and table scraps, especially fatty foods, can increase the risk for pancreatitis. Make sure to avoid giving these altogether.
As an example, recently my young son asked me if he could give his hound dog a piece of bacon from his breakfast plate. “No way!” I gasped. “That is pancreatitis waiting to happen!”
As I cautioned my son, we must resist the temptation to share love in the form of human food with our four-legged family members. Of course, the temptation is heightened during the holidays when our celebrations often revolve around feasts and special tasty treats. It is important to stay strong, though. Not only is pancreatitis a possibility if you share fatty foods with your dog, but also some holiday foods are dangerous for dogs.
Finally, if you do need to switch your dog’s diet, remember to do so gradually over five to seven days to reduce the risk of GI upset or pancreatitis.

3. Obesity increases the risk of severe pancreatitis.
It is important to keep your dog at a healthy weight for many reasons, including the fact that obesity increases the risks that your dog will develop severe (and sometimes fatal) pancreatitis. To learn whether your canine companion is overweight, start by determining your dog’s body condition score. Then, if you decide some weight loss is in order, partner with your vet to determine how to help your dog lose weight.
4. Endocrine disorders may increase the risk for pancreatitis.
Your dog’s endocrine system is responsible for the regulation and release of numerous hormones, many of which can affect the pancreas. Diseases associated with the endocrine system like Cushing’s disease in dogs, hypothyroidism in dogs, and diabetes in dogs increase your dog’s risk for developing pancreatitis.
5. Some medications may contribute to pancreatitis.
The use of certain medications can increase the risk of canine pancreatitis. These include:
- Immunosuppressive drugs like azathioprine.
- Medications used to treat seizures in dogs like phenobarbital and potassium bromide.
- Antibiotics like sulfonamides and tetracycline.
- Certain diuretics (medications to help remove excess fluid from the body).
- Chemotherapeutic drugs like L-asparaginase.
If your dog is taking a medication long term and is experiencing pancreatitis symptoms, make sure to contact your veterinarian.

6. Toxins can cause pancreatitis in dogs.
Certain toxins, such as zinc and organophosphates can also potentially cause pancreatitis.
Dogs tend to get zinc toxicity if they swallow a zinc-containing object such as US pennies minted after 1982, nuts and bolts, board game pieces, zippers or snaps, etc. Or they may eat zinc supplements, diaper cream, or other zinc-containing medications.
Organophosphates can be found in some home, garden, or agricultural insecticides. Exposure can be through ingestion, inhalation, or contact with the skin. Initially, organophosphate toxicity causes signs like vomiting, diarrhea, excessive salivation and tearing, urination, muscle tremors, or seizures. However, afterward the dog may also develop pancreatitis.
7. Injury, cancer, and bacteria are other factors which may increase the risk of pancreatitis.
Infections rarely cause pancreatitis in dogs, but there have been reports of certain bacteria causing pancreatitis. Trauma and physical injury can also trigger inflammation of the pancreas. Additionally, dogs can develop cancer of the pancreas, which may manifest as pancreatitis.
How does a vet diagnose pancreatitis?
Diagnosing a dog with pancreatitis involves using the symptoms, history, and diagnostic test results to determine if pancreatitis, or another condition, is the most likely culprit.
Gathering a history
When you bring your dog with pancreatitis symptoms in for an exam, the vet will often start by asking questions about your dog. Gathering a complete medical history is often just as important as running the diagnostic tests when it comes to diagnosing pancreatitis in dogs.
Tips for the history portion of the exam
To help you provide your vet with the necessary information, keep these three tips in mind:
- Make a list of foods your dog has eaten. Check with family members to see if your dog has consumed any human food, eaten out of the garbage, or even counter surfed any foods, especially high-fat foods like pork, beef, or bacon.
- Keep a record of your dog’s symptoms. How many times did he or she vomit? What did the vomit look like? Is he or she still eating and drinking? When did the signs start? Is he or she getting worse, better, or staying the same?
- Plan for your veterinarian to ask for your dog’s history. Knowing your dog’s past history is especially important if it is after-hours for your regular vet so you are going to an emergency veterinary clinic.
Running diagnostic tests
Definitively diagnosing pancreatitis can sometimes be challenging. This is because other factors can affect the accuracy of the tests. As part of the work up, the vet may run the following tests:
Chemistry panel and complete blood count
The vet may start with some basic blood tests for dogs. If your dog has pancreatitis, the chemistry panel might show elevations in certain enzymes like amylase and lipase. However, other illnesses besides pancreatitis may affect these numbers.
Additionally, some dogs with pancreatitis have high liver enzymes in dogs, elevated kidney values and cholesterol, and changes in electrolytes and proteins. On the complete blood count (CBC), dogs may have elevations in neutrophils (a type of white blood cell), anemia in dogs, or low platelets in dogs. None of these findings are specific to pancreatitis, though.
Abdominal ultrasound
Since the pancreas is tricky to visualize on X-rays, an abdominal ultrasound is much better for evaluating it. However, up to one-third of dogs with pancreatic inflammation may have normal findings on abdominal ultrasound.
Canine pancreatic-lipase immunoreactivity (cPLI)
The cPLI is probably the most useful test for pancreatitis. It looks at the levels of pancreatic lipase in a dog’s blood and is available to veterinarians as a 10-minute in-house test or a test that can be run at a diagnostic laboratory.
If the test is negative, then pancreatitis is unlikely. If the test is positive and your dog is showing clinical signs, then it is likely that he has pancreatitis. However, false positives and false negatives are possible. Thus, the vet will interpret cPLI in light of the history, symptoms, and other findings.
Fine needle aspirate of the pancreas
While not currently a common diagnostic tool, a fine needle aspirate (FNA) of the pancreas (using a small needle to retrieve cells from the pancreas, which are then examined under the microscope) can also help diagnose pancreatitis. In a study of 92 dogs who underwent pancreatic FNA, it had a good diagnostic yield (provided a diagnosis 73% of the time) and low rate of complications.
Additional tips for the visit itself
When at the vet clinic for the appointment, the following four tips can help you have realistic expectations:
- Know that your vet may recommend blood tests, X-rays, or an ultrasound. These tests assess your pet’s overall status and can help distinguish pancreatitis from other similar-appearing conditions.
- Take a deep breath and mentally prepare yourself for the time it may take to complete the testing. Sometimes the vet may start with one test, then recommend another once he or she has evaluated the results of the first test. This is all part of the diagnostic process.
- Prepare yourself for potentially spending some time away from your dog. Pancreatitis can be very serious and even life-threatening at times. Your vet may recommend hospitalizing your dear dog for additional care and observation.
- Know that you may be referred to an emergency clinic, especially if your vet thinks your dog needs critical treatment that is beyond the scope of what a general practice can provide.
What is the treatment for pancreatitis in dogs?
After reaching a diagnosis of canine pancreatitis, the vet will discuss the treatment plan with you. It may involve:
Fluid therapy
Fluid therapy is an important part of treatment because it helps correct dehydration, keep up with fluid loss from vomiting, and supply fluid to keep up with normal daily requirements. Sometimes in mild cases, your vet can administer fluids under your dog’s skin (subcutaneous fluids for dogs) and send him or her home with you.
However, many cases of pancreatitis will require hospitalization for IV (i.e. intravenous or in the vein) fluid therapy. This is one of the mainstays of pancreatitis treatment.
Anti-nausea medications
To reduce the nausea your dog is experiencing and keep him or her from continuing to vomit, the vet will typically administer anti-nausea medications. Cerenia for dogs (maropitant) has become popular with many vets for the treatment of pancreatitis because in addition to being an anti-nausea medication, it is believed to have some abdominal pain-relieving properties.
Pain medications
The vet will use pain-relieving medications to decrease abdominal pain and keep your dog more comfortable. Generally, vets prefer opioid medications over non-steroidal anti-inflammatories (NSAIDs). Keep in mind that even if your dog is painful at home, you should never give him or her any human NSAIDs or other human pain medications. Instead, consult with your vet.
Special diet
Feeding a low-fat, highly-digestible diet can help keep the GI tract moving and restore the dog’s appetite. The low-fat component is important because a high-fat diet is a risk factor for pancreatitis. Some dogs will need to stay on a low-fat diet for life. Your vet can advise you about what to feed a dog with pancreatitis, both in the acute phase and long term.
PANOQUELL
Previously, the only treatment for pancreatitis was supportive care. But now we have PANOQUELL®-CA1 (fuzapladib sodium), an exciting new drug that is aimed specifically at managing pancreatitis and the associated symptoms. It works by stopping neutrophils (white blood cells which are a major driver of pancreatic inflammation) from entering the pancreas and releasing inflammatory molecules. The end result is less pancreatic inflammation and therefore a reduction in clinical signs.
PANOQUELL is administered as an intravenous injection once a day for three days. It is intended to be used in conjunction with other standard treatments for pancreatitis (fluids, anti-emetics, diet change, etc.). In studies conducted by the manufacturer, dogs who received PANOQUELL plus supportive care recovered more quickly than those who just received supportive care.
Steroids
While controversial, some vets will choose to use steroids such as prednisone for dogs in situations where the dog is severely ill and not responding to traditional therapy.
Surgery
Occasionally, a dog may need surgery if bile flow is obstructed or there is a pancreatic abscess or pseudocyst (walled-off collection of pancreatic secretions).

Can supplements be used to prevent or manage pancreatitis in dogs?
Understandably, many of my clients ask me if there are any supplements, or other good options for decreasing their dog’s chances of developing pancreatitis. Unfortunately, there aren’t any supplements that look very promising at this point.
Some studies in humans with pancreatitis indicated that supplementation with pancreatic enzymes made people feel better but didn’t change the level of inflammation. At this point, we don’t have a lot of evidence to say that pancreatic enzyme supplementation will benefit dogs who are prone to pancreatitis but still make enough pancreatic enzymes on their own. Dogs with exocrine pancreas insufficiency, however, do benefit from pancreatic enzyme supplementation.
Antioxidants have also been proposed as potentially beneficial in people (and therefore possibly dogs) with chronic pancreatitis. However, researchers have not identified the best antioxidant combination or product yet. Some people have also tried probiotics in hopes that balancing a dog’s gut flora will decrease the pancreatitis risk.

How can you decrease the risk of your dog getting pancreatitis?
Since the jury is out regarding supplements, I usually tell my clients to focus on the things that we know can make a difference—your dog’s diet and weight. As discussed in the treatment section, your vet may recommend continuing to feed a low-fat diet even after your dog has recovered from the pancreatitis episode. This, in conjunction with being extremely vigilant in preventing your dog from eating anything other than his or her dog food, can make a big difference.
Additionally, if your dog is overweight or obese, work with your vet or a veterinary nutritionist to formulate a weight loss plan. Not only will being at a correct body weight reduce your dog’s pancreatitis risk, but it will also decrease stress on his or her joints and organs. Overall, weight loss is a win-win situation for everyone.
Finally, if you think your dog has pancreatitis, the most important thing you can do is to get him or her to the vet ASAP. Don’t waste time trying home remedies or taking a wait-and-see approach. Pancreatitis is serious and can be life-threatening.
What is the prognosis for dogs with pancreatitis?
Dogs with mild forms of pancreatitis who respond quickly to treatment have an excellent prognosis. However, dogs with more significant symptoms may take longer to respond to therapy or need more intensive care.
Dogs with severe pancreatitis, pancreatic cancer, or necrotizing pancreatitis (where part of the pancreatic tissue has died), have a guarded to poor prognosis. Unfortunately, some dogs with severe pancreatitis die or are euthanized due to life-threatening complications like multi-organ failure, shock, or disseminated intravascular coagulation (DIC).
Since pancreatitis in dogs is not contagious, you don’t have to worry about it spreading to your other dogs. But you do need to get help for your sick dog quickly. Like almost every medical diagnosis, there is extreme value in early detection and treatment. Make sure to contact your veterinarian right away if your dog ever has signs of pancreatitis.
The rest of my Miniature Schnauzer patient’s story
Are you wondering how things turned out for my Miniature Schnauzer patient? As I talked with Ellie’s mom, I learned she had been stealing some food from the new dog’s bowl over the past week. Also, her “grandma” had come to stay at the house and was feeding her table scraps every night at dinner.
One plus one usually equals two. My patient was exhibiting classic signs and had eaten human foods, which made me immediately suspect pancreatitis.
I promptly hospitalized her and started her on intravenous (IV) fluids. She also received injectable pain medication and anti-nausea medication. By the following day, Ellie had perked up and was eating dog food on her own!

When I saw my patient at her progress exam a week later, she was back to her bouncy self. Because she was a Miniature Schnauzer, a breed prone to hyperlipidemia (i.e. high fat levels in the blood) which can be a pancreatitis risk factor, I prescribed a low-fat, canned diet which she continued to eat long term.
Be proactive about pancreatitis prevention and treatment
By sharing this dear dog’s story, I hope that proactive dog owners adopt a “just say no” policy about sharing temptations with dogs. While some dogs may be able to handle abrupt diet changes or a high fat meal, the potential for pancreatitis is not worth the risk.
I don’t want you to think, though, that you did something wrong if your dog gets pancreatitis. Sometimes it may happen despite your best efforts because not all risk factors are in your control.
If your dog does seem to be showing signs of pancreatitis, seek veterinary care promptly. Pancreatitis can be dangerous, so the sooner your vet can address it the better. Hopefully, due to your quick action, your dog will be back to normal again soon, just like my patient!
Do you have questions about pancreatitis in dogs?
Please comment below. We can all learn from each other.
This post was originally published on June 7, 2021 and updated on May 5, 2025.


Thank you for a very informative article. My one year old lab/weimaraner mix has been tested for pancreatitis but was negative. Can you tell us what kind of low fat canned dog food you would recommend? Thank you.
Hi Nicole,
There are several brands of dog food that make a low-fat variety in cans. I have had good success with Purina EN Gastroenteric Low Fat, Hill’s Digestive Care I/D Low Fat, and Royal Canin Gastrointestinal Low Fat. I am curious to know why you are looking for a low-fat food for your pup if the pancreatitis testing was negative? I would not recommend using a low-fat food if it isn’t medically necessary as this could lead to other unexpected issues for some dogs. If you have any lingering concerns or questions, don’t hesitate to reach out to your vet. They should be able to offer advice and guidance. Bless you and take care!
Dr Buzby- just came home from the vet. My boy Rex was diagnosed with pancreatitis. He received 3 injections and medications I have to administer. They did not give him an IV, no pain meds, and the vet stated he has to come back daily for shots tomorrow and Saturday. Poor little guy constantly vomits, but today he started vomiting blood. I freaked out, left work immediately in the middle of a client meeting and drove he and his Brother to the vets office. They are both American cocker spaniels aka love bugs. How will I know if he has chronic pancreatitis.? What are the next steps to ensure he recovers and his brother does not get pancreatitis? Will his brother get it? Your page is so helpful!! I will no longer be giving them people food!! I am also going to check all of the labels on their treats and dog food!
Hi Tracey,
I am sorry Rex had to endure this painful condition. I am glad your vet started treatment quickly and hope he responded as expected. The word “chronic” refers to a long period of time. So, if this one pancreatitis episode starts to turn into an ongoing issue, then your boy would be classified as having chronic pancreatitis. Your vet will be able to guide you through the recovery process and offer ways to hopefully prevent any further issues from developing. Diet can play a big role in whether the pancreas becomes inflamed again or not. Luckily pancreatitis is not contagious, but if your other pup is truly a genetic “brother” then he may be at a higher risk for developing something similar. How is Rex today? Praying he has made a full recovery and wishing him all the best of luck for many happy days ahead.
Our 12 year old Catahoula mix, Tiberius, has been having issues with vomiting occasionally (usually around 5 hours after eating) and having stools that run the gamut of soft but formed, soft and unformed, and watery diarrhea for the past couple of months. For the past 8 months or so he would vomit less frequently, maybe once every couple of weeks, but no stool issues. Upon a vet visit last month to address the gut issues our vet had the blood panel done and found that the ALT was 241, the ALP was 180, but the other two liver numbers were in the normal range. Tiberius had slightly elevated pancreas PSL number at 142, just 2 over the top range. Our vet gave Tiberius metronidazole for his diarrhea (which I didn’t know until I researched it was an antibiotic), denamarin for the liver, and a low digestible dog food to try. Tiberius is still suffering from vomiting (2x last week and once this past Monday) and his stools are unpredictable, one movement will be very nearly solid and the next three are nothing but watery diarrhea. We started him on Cobalequin for vitamin B12 and our next step is to try a pancreas enzyme, as our vet gave us those as options if the prior things we tried didn’t help. Tiberius still has a good appetite and doesn’t seem lethargic; I don’t know what is causing his gut issues and what to do to get them back to a more normal state. I have been researching this and I am so glad that I found your website this morning. You write in a detailed way so that it is easier to try to determine what may be or may not be going on with our pets, and I appreciate it.
Hi Sandra,
I am sorry Tiberius is having these chronic GI issues. I am glad you found the article to be helpful and appreciate the positive feedback. It sounds like your vet is working their way through the diagnostic process and is being proactive and thorough. Don’t forget you can always ask about a consultation with an internal medicine specialist if needed. Hoping you were able to get some answers and find the best treatment for your boy. Feel free to leave an update and let us know how things are going. Wishing you both the best of luck and praying for healing.
My 10 year old Pomeranian was just diagnosed with diabetes , high keytones and pancreatitis. She vomited a few times and stopped eating so I took her to the vet. They did fluids and insulin sent her home for me to return in the morning for another day of iv fluids (they are not open 24 hours) doing this for 3 days. The keytones went down and so did blood sugar. She still will not eat or drink on her own and is very lethargic and can not stand . Is this normal when being treated and getting to recovery?
Hi Samantha,
I am sorry your senior girl is not feeling well, and I understand your concern. With so many issues occurring at the same time, I am not sure there is really a “normal” way for things to progress. In tough situations like this, you have to remain steadfast with treatment and give things time. Changes to your pup’s treatment protocol will depend on how her body responds and your vet will take it day by day (sometimes hour by hour). Hoping you will start to see things stabilize soon and praying for a positive outcome. Best wishes to you and your sweet girl.
Hi,
I took my little girl to the vet this past Saturday. She was anxious on Friday night and didn’t eat at all on Saturday. She was extremely lethargic and movement wasn’t great. She is 13 and has been on Galliprant due to mild arthritis. The vet took blood and urine tests; including one for pancreatitis.
She also gave her a shot of Librela, thinking that would help the joint pain and mobility issues.
It seems she got worse and I took her to the vet this morning. She was not eating at all and couldn’t stand on a non-rug service. I did a search of Librela online, which of course was the worst thing to do.
The vet was fairly confident it wasn’t the shot. The blood work came back and the indications were very high for pancreatitis. She started her on IV for hydration along a nausea reliever and an antibiotic. She will stay overnight at the vet and may need another night, depending upon response.
If response tomorrow is not great, she recommends an ultrasound of her tummy to ensure it’s not something really serious.
She wasn’t vomiting and she didn’t have diarrhea. Fever is slightly high.
This all has me freaking out.
What do you think?
Thank you!!
Hi William,
I am sorry your girl is so sick, and I understand why you are worried. I think your vet is making the right calls and that an abdominal ultrasound is a good next step. Pancreatitis can be very serious and the symptoms you describe sound like a typical case. I hope the IV fluids and hospitalization will help to get things turned around. Wishing you both strength and comfort as you navigate this difficult road. Praying for a positive outcome!
my Mastiff Zeke was diagnosed with pancreatitis and spent the night in the hospital for fluids and meds. he has separation anxiety so we decided he might do better at home. he was initially seeing the vet for back leg weakness and they did bloodtests that showed pancreatitis. he has progressively gotten worse with mobility. he has taken a small amount of pumpkin today with no vomiting . I’m really worried about his back legs, he has actually fallen to the ground and unable to get himself up..(he is 130 lbs)
Dear Kathi,
I am sorry Zeke is not doing well and I understand why you are concerned. Without examining him myself, it is hard to give you advice about how to proceed. Please make sure your vet is aware of this ongoing mobility issue. They may have thought the hind limb weakness was due to the pancreatitis and that may be true. But I also don’t want there to be something else contributing to Zeke’s problems that we are missing just because we haven’t investigated thoroughly enough. With giant breed dogs, a lack of mobility can lead to a very poor quality of life. I think this needs attention sooner rather than later. Praying for answers and a clear path forward. Wishing your sweet boy all the best hoping he can make a full recovery.
Thank you for publishing this important information. My dearly loved 6 year old dog had chronic pancreatitis. It went undiagnosed for a long time, as his symptoms were not typical. I would warn everyone to be vigilant about any time your dog throws up. My dog Eddie, would regurgitate his food soon after eating (then quickly re-eat the food), about once a month, until I started feeding him in smaller increments, which stopped the regurgitation / vomiting. He began licking his penis incessantly and when I took him outside one evening soon after this began, he lifted his leg to go potty and fell over. He didn’t want to get up, so I picked him up and brought him into the house, put him on the sofa to relax. About 30 min later, he was up and around and wanted his dinner. The next day I took him to the vet, described what had been going on and they did a urinalysis and said he had a bladder infection. Antibiotics were prescribed. About 3 days after the course of antibiotics ended, the licking came back, I called the vet and they gave more antibiotics. Same happened after the next round of antibiotics, so I called again. They told me my dog had a nervous disorder and was licking himself to self soothe. Said to keep a cone on him and keep him calm. If I wanted, they could prescribe prozac for dogs. I did not want the prozac, as I wasn’t convinced he had a nervous disorder but I did work to keep him calm and tried to keep a cone on him, which he didn’t really like. He was eating well, not vomiting so I thought we were working through whatever this was. In a couple of months, the licking was incessant, and I could not keep a cone on him. His fur had started to change color — from jet black to each hair follicle being tan next to his body and black on the end. I took him to the vet and described what had been going on, he prescribed a skin antibiotic and steroids, did a light treatment on his private area, and prescribed ‘calming care’ supplement. I was worried this wasn’t the issue and said to the vet that I didn’t think he had a nervous disorder, it wasn’t just a skin issue, it was something else. He sent us home. The situation got a bit better, but then he started licking a different area, I took him back in and demanded a full blood panel. The results showed elevations in some areas, where the vet said he wanted him to have a cushings stim test. I got a copy of the blood work and it suggested next step was a urinalysis, so I brought in a sample, as they didn’t have any appts open. They told me his urine wasn’t concentrating. I didn’t know what that meant, and they told me to bring him in for the stim test, which I did the next week. The stim test showed he did not have cushings disease, so I asked what are the next steps to address the urine not concentrating and the elevated blood values, they told me to restrict water, which I did not do, as I had been complaining to the vet that he hardly ever drank water in the first place and I was trying to sneak water into his food to help the dehydration. They also said they would prescribe supplements for the elevated liver values. The next day, little Eddie got up to go outside an threw up about 1 tablespoon of clear liquid on the top step outside, He came back in. After a couple of hours wasn’t feeling well, seemed not himself. I tried the emergency vet (this was Saturday and all the local vets were closed) and the er vet was also closed. I live about 150 miles from the next ER vet hospital, so since he only threw up once, got a relatively good report from the vet the day before and further he was a nervous car rider, so I didn’t want to get him all riled up for that long when not feeling well, I thought we would wait until the evening to see if the local ER vet opened that evening, as sometimes they open at 6pm. They did not open. Eddie got up on the sofa on his blankets and he and I fell asleep, I awoke at 1am and he was gone from the sofa and had messed the blankets, which was unusual for him. I found him on the floor next to the sofa, unconscious. I tried to wake him and he was not responsive. He started to have seizures and I was in a panic. I finally found a vet a few towns away that opened at 9am on Sunday. I held him as I drove to the only vet I could find that was open. They diagnosed him with acute liver failure and pancreatitis. He then soon went to the emergency vet and was diagnosed with Hepatic Encephalopathy. Two days later, It ended up killing him. I am devastated. No one would tell me how this all happened so quickly and what caused it all to occur in the first place, so I got copies of all his blood work/ urinalysis info and pieced the puzzle together myself after doing a lot of research. His blood and urine results confirmed a very high probability he had a blocked bile duct. I investigated the causes of a blocked bile duct, liver failure and HE and found that chronic pancreatitis was the common element behind all of it; it is a cascade of horrors. Chronic pancreatitis doesn’t have typical symptoms in all cases, and didn’t cause loss of appetite, lethargy, or even vomiting in my dog. I assume the licking of his penis was more licking a very tender / sore abdomen and had nothing to do with his privates. All the limited symptoms he did have would pass in a couple of hours, except for the licking of his privates. Brewing under it all, chronic pancreatitis was there. He had never had acute pancreatitis in the time I had him, so being a rescue dog, you don’t know their history. I assume the cPLI test would have detected it earlier, but unfortunately, it was not included in a ‘full blood panel’ that I requested. I had assumed “full blood panel’ meant they checked these things, but that was incorrect. For something as known as pancreatitis, I wish vets would automatically include the pancreatitis check in all “full blood panels’ when a client requests a full blood test panel. We, as pet parents, do not know what is / isn’t included in tests and so we can’t ask for things we aren’t aware need to be asked for separately. I am heart broken my 6 year old beloved Eddie had to pass away due to something that was treatable, had it only been diagnosed. I brought him to the vet, but it was repeatedly missed. Since, I have gotten better at reading blood and urine tests, I know what to look for in their poop,etc. Please everyone, look into their blood tests / urinalysis and do some research using the IDexx site, Merck manuals, NIH site so you have some idea what is going on with your pet. Vets, especially since the pandemic, are busier and there are fewer of them, so it is on us to help fill that gap. I so wish I had done more, earlier and asked more questions. I feel strongly that things could be very different right now, had I only done more. My heartbreak is unrecoverable.
Dear JoAnne,
I am so sorry for your loss of Eddie. It is clear he was dearly loved, and I can only imagine how much you miss him. It is hard to work through grief when left with more questions than answers. I understand why you have done such extensive research and agree that knowledge is power. Ultimately, you may never know for sure exactly why things progressed the way they did for your sweet boy. But I hope you can take comfort in knowing he lived a happy life, and I am certain he knew how much you loved him. Praying for peace and healing for your heart. May Eddie’s memory stay with you always and bring you joy.
Thank you Dr. Buzby. I am not sure I will get over the loss of my beloved little Eddie. He was very special to me and I needed him to be with me at least another 12 years. Robbed of our life together.
Thank you for the good work you do to help spread important information to pet parents. It is vital people take heed and get involved in their pets care. I typically do, but Eddie was so special to me, and one of the vet techs scolded me for “googling” too much about my dogs, so that made me take a step back with Eddie. Sadly, this is the outcome of stepping back. Like so many, I desperately want to turn back time and get another opportunity to do things the way I should have.
Thank you JoAnne for sharing your story. And thank you Dr. Buzby for providing this informative sight for all of us animal owners.
I am so sorry to hear of your beloved, Eddie. It seems no matter what we do. It is hard not to feel we could have or should have done more.
I lost my beloved 12-1/2 year old pug, Louis this past weekend to acute pancreatitis.
He first presented with symptoms 2-1/2 weeks before he passed. Drinking a lot of water. But, when he drank water. He tended to drink a lot at one time, his entire life. I did pay attention to him peeing outside though. It looked normal color. We always had pads around the house because he was older. He did start using them more than usual. I didn’t notice any unusual smell or color in his urine or poop.
A few days after this, he threw up for the first time. He continued with a strong appetite though. Eating his breakfast and lunch. As well as drinking water. Then over the course of the next few days. He would throw up once or twice a day. And he seemed lethargic. I was thinking due to throwing up. I still felt like something was wrong though. So I took him to the vet. They did a blood workup on him and detected high liver enzymes. That was the only thing they saw wrong in his bloodwork. They suspected a liver function issue or gallstones due to his age. Pancreatitis was never even mentioned. He was prescribed Denamarin and Ursodial for his liver. Cerenia for nausea. Amoxicillian and Metronidazole antibiotics and sent home.
He took these with chicken and rice. He continued to eat and drink water. He went to the bathroom outside, pee and poop looked normal, did not have an unusual smell. But on the fourth day of taking meds. He did not want to eat. So we crushed the pills and put them in a syringe of water. Which he took.
I did not like any of this at all. Plus he was very lethargic. So we took him back to the vet the next morning. I chose a different vet at the office. This time we got an ultrasound done as he was not getting better. He was diagnosed with acute pancreatitis. He was put in the doggie ICU with full meds and IV. I of course told the vet to give him everything he needed to try to survive this. He was given an aggressive treatment plan. Too much to list here. His liver enzymes would not go down though.
On day four he seemed to be responding to the meds. His eyes were clearer and he was active and responsive in our visit with him. His personality was there as well.
But, early in the morning on day five. He stopped breathing. They tried CPR to no avail. They suspected organ failure. The vet said he had a lot working against him. Age, not eating solid food for several days and the liver enzymes that were not responding to treatment.
I have done nothing but question every decision I made with him over the course of the last few weeks. Wondering if there was anything I could have done sooner? Would aggressive treatment have made a difference if started sooner? It all seemed to happen so fast. Barely three weeks went by from the first time I noticed anything unusual with him, till his death.
JoAnne, your story touched me and made me feel not so alone as I have felt. I do hope that by reading this. You do not feel as alone in your grief as well. And that the passage of time since December has softened your grief.
Sending blessings of comfort to you and your dear, Eddie
Dr. Buzby, if you have any thoughts on my situation to share. I would appreciate it.
Dear Larry,
I am so sorry for your loss of Louis. My heart aches for you with all you have endured over the past few days. It is normal to ponder all the “what ifs”, but please don’t carry the unnecessary burden of guilt for how things progressed. Pancreatitis can turn into a serious situation very quickly even if the appropriate treatment is being administered. Even if you had been able to get a diagnosis days earlier, there is no guarantee that the outcome would have been any different. You didn’t do anything wrong, and you certainly did not fail your boy. I hope with time your heart will begin to heal and the grief will fade. May the memories of all the good times you shared continue to bring you joy. Louis will never be forgotten. Bless you. ♥
my dog Chewy was just diagnosed with pancreatitis.. he was hospitalized for 2 days sending him home at night, it sounds like they have done everything you are suggesting as far as the IV medications, his abdomen is very sensitive and I believe this is going to take some time to hopefully get under control, he is a 20 pound Lhasa Apso on ID low fat canned prescription food and I believe the treats and roast beef table scraps were the culprit he wouldn’t eat for almost 3 days I finally got him to eat boiled chicken NO seasoning at all but he finally ate it what kind of rice should I add to it and I’m also going to add some pumpkin is this better than the canned dog food? we have cut out EVERYTHING else, we were sent home with gabapentin , tramadol, Cerenia,proviable caps, and entyce, and Diagel, but his diarrhea is under control ,he was given fluids ,and pain medication by IV and I believe another drug I’m not sure what it’s called, I’m scared to death, I know he isn’t feeling good but I do see improvement, is the fresh boiled chicken better than the prescription low fat canned food, his stools are soft but not runny, and urinating normally I’m watching every move, how often is this cancerous and should I get an MRI, my vet tried explaining the special blood tests and what was elevated telling her she believed it is pancreatitis, but not able to say whether it is cancerous?
Hi Connie,
What a concerning few days you have had with Chewy! I’m glad he seems to slowly improving each day. In terms of your questions about his diet, the most important thing for the next few days is that he is eating something that is easily digestible and low fat. It doesn’t matter so much whether it is I/D low fat or boiled chicken and plain white or brown rice. However, if your vet thinks that he should be on a low fat diet long term, the exact nutritional composition of the diet matters more. In that case, you would probably want to either have him on the I/D low fat or work with a veterinary nutritionist to ensure that you are feeding him a balanced homecooked diet. I’ll include links to two articles below that may be helpful for you.
I’m not quite sure I’m following your other question, but often pancreatitis is triggered by a high fat meal (maybe the roast beef like you thought) rather than cancer. However, since I didn’t examine him or look at the bloodwork, I can’t give you specifics about if you should pursue further testing. Checking in with your vet or having an appointment with a veterinary internal medicine specialist should be able to address those concerns though.
I hope your sweet little guy makes a full recovery and that you are able to have a fruitful and reassuring discussion with your vet (or a specialist) about the next steps for him.
Here are the articles I mentioned:
1) Bland Diet for Dogs: What, How, and When
2) What to Feed a Dog With Pancreatitis—According to a Vet
Thank you for your informational articles! Our 2 senior border collies LOVE peanut butter. I usually put it on licki mats or other similar treat toys and freeze. I’ve done this for years and they do not have any digestive issues. But now I’m a bit worried that it could cause pancreatitis. If they have been fine with peanut butter for years (weight and digestion are good) do you think it’s ok to continue this treat? Thank you!
Hi Beth,
I use peanut butter frequently to get my own dogs to take pills. While any food can cause issues, I think you are probably ok to keep using this as a treat (everything in moderation). As always, please discuss this with your vet since they are more familiar with your dogs’ specific needs. Thanks for reaching out!
Dear Dr. Buzby,
My 16 year old Basset Hound suffered a mild case of acute pancreatitis the same week she was diagnosed with a UTI. She is a slim and trim for a Basset Hound and only had abdominal pain which made it challenging to diagnose. It was not until an ultrasound was performed that we had the diagnosis of pancreatitis.
I am used to feeding her holistic/healthier foods and am now finding it challenging to find her fresh frozen and/or raw food that stays under 30% Metabolic Equivalent (ME) of fat OR lower than 15% fat on a dry matter basis. I have even contacted several of the higher end dog food companies about this issue with no luck.
When looking at the prescription vet diets, I was not at all impressed with the ingredients. Is there a such thing as a healthier/holistic prescription vet diet for pancreatitis as some of the common ones don’t look very healthy when I review the ingredients. I thought I would ask you since you seemed to be more holistic minded when I read your articles. Our Basset Hound also wears your toe grips 🙂
Thanks for any advice on this,
Sincerely,
Ingrid
Hi Ingrid,
I am sorry your Basset has had such a tough time the past few weeks. Glad to hear you were able to get a diagnosis and start treatment fairly quickly. Here is a link to another article that discusses food recommendations for dogs with pancreatitis in more detail: What to Feed a Dog With Pancreatitis—According to a Vet
You will probably want to scroll down and take a look at the paragraphs titled “Homecooked low fat diets” and “Pre-made homecooked low fat diets”. I hope this will be helpful and get you headed in the right direction. How is your girl feeling today? Praying she is on the road to a full recovery. Best wishes to you both!
My dog was diagnosed with pancreatitis 2 weeks ago no appetite.. vomiting.. diarrhea.. she spent a week in the hospital .. been home 5 days .. has taken her meds and was given a low fat dog food. Vomiting stopped for a couple of days .. has since started vomiting again diarrhea has continued getting very wet and dark with a strange smell.. she want to stay under the sofa. Comes out occasionally for a drink , urinate or diarrhea. I’m at a total loss
Hi Anne,
I am very concerned about the symptoms you are describing. It sounds like your pup may have relapsed and could need attention from your vet right away. I highly recommend you call your vet and get your dog evaluated as soon as possible. Praying she can overcome and make a full recovery.
Hello everyone
I have a question will a dog have bloody loose stools from pancreatitis?
Thank you
Ps. Our Dog was taken to a Vet that was unfamiliar with him.
Our dog had no previous problems just started to pass bloody stools and wasn’t eating well.
They didn’t do an ultrasound and I read some blood tests can mimic pancreatitis but be other…
They sent him home
I’m looking for some answers…
I seen the chicken, rice, pumpkin…
I’ll try thank you
Hi Tamara,
Yes, pancreatitis can cause bloody diarrhea. There are some abnormalities that can be seen on bloodwork that could make a vet suspicious about pancreatitis without giving a definitive diagnosis. But there is also a snap test that can be done in the clinic that can help with a diagnosis. If you need a second opinion or have lingering concerns, it might be a good idea to have your dog evaluated by a specialist. I hope you can find the answers you need to make sure your pup is on the road to recovery. Praying for things to resolve quickly. Wishing you both the best.
Our mini Aussie (just turning 14) suddenly experienced ongoing diarrhea. Our vet has diagnosed pancreatitis. We were feeding her low fat dog food but the diarrhea persisted. We are now feeding her chicken and rice but she seems famished all the time. Adding pumpkin to her diet seems to have helped reduce the diarrhea to a soft but manageable stool. But she has lost 4 pounds over about three months. Any suggestions? What can an ultrasound tell us? Thank you.
Hi Penny,
I am sorry you are having such a difficult time finding the right food for your Aussie girl. Pancreatitis can be very tricky and take a while to completely resolve. An ultrasound can give you a better picture of what is happening in the abdomen. It might be able to tell the difference between inflammation or a possible tumor/cancerous process. If the diarrhea is persisting, then an ultrasound could be the best next step to figuring out a solution. Also, you may want to think about a consult with a veterinary internal medicine specialist. I hope you girl is feeling better quickly and can get back to living her best life. Best wishes to you both.
My mini Aussie is currently in the hospital being treated for pancreatitis. He had a small amount of “leakage” in his abdomen. How does this happen? If it is caused by a leakage from the pancreas can this heal/repair? Also, what I have read says how soon they get treatment is critical. He started vomiting Thursday in the early morning (middle of the night) and I took him to ER Friday evening. Was sent home with meds but he couldn’t take them. Took him back to ER Saturday night and they kept him to run more tests. How soon is soon enough? I am so worried. Doc said he was able to eat a little on his own today.
Hi Kim,
It can be so scary when a beloved dog is in the hospital. Sorry to hear you are currently facing this with your mini Aussie. Since I can’t examine your dog or look at the diagnostics, I can’t confidently comment on what “a small amount of leakage in his abdomen” means for your pup. Sometimes vets may use this phrase to mean several things. However, I’m sure that the vet is treating your Aussie would be happy to give you a better idea of what he or she meant and how this changes your dog’s prognosis. It sounds like you did a good job of getting him to the vet to start treatment. A lot of the time they do respond to outpatient treatment like you started on Friday but not always (and there isn’t a good way to have predicted this). Good job on advocating for him and bringing him back to the ER when he wasn’t able to take the meds. It sounds like he is in good hands. Hopefully he will be on the mend soon! ❤
This came at just the right moment. My lab Dolly has had pancreatic problems for 6 months, I did all the wrong things, too many treats, licking pots and pans, etc, and she is paying the price. Our wonderful vet has prescribed all the right meds and food (canned EN ) and low-fat prescription kibble. She was treated with hydration therapy but still the pancreas hasn’t healed so she is getting an ultrasound on Thursday.. We hope it is not cancer. She wears her toe grips because of severe arthritis and bless her heart, she is always one happy girl, tail never stops wagging. Thanks for the information. One question, does laser help the pancreas and the tummy pain? She gets laser therapy for her joints two to three times a week and maybe we should use it on her tummy. I appreciate any feedback
Gale Blanchard
Hello Gale, Many thanks to Dolly for being a ToeGrips Ambassador! I’m so sorry to hear of her issues with pancreatitis. To answer your question–No, typically we don’t use laser to treat this condition. The ultrasound should be very helpful in getting to the bottom of this. She will probably be on a prescription diet for life. I hope this is behind you soon and Dolly recovers completely!♥️