If you heard your vet say “kidney failure in dogs” and everything else he or she said about your senior dog’s diagnosis was a blur after that, this article is for you. Integrative veterinarian Dr. Julie Buzby explains kidney failure in detail—what it is, the types, symptoms, common causes, which tests your vet may run, the various treatment options, and the overall outlook. Armed with this information, you will be ready to navigate kidney disease with your dear dog.

- What is kidney failure in dogs?
- Where are a dog's kidneys? What do they do?
- What are the types of kidney failure in dogs?
- How fast does kidney failure in dogs happen?
- What causes acute kidney failure in dogs?
- What causes chronic kidney failure in dogs?
- What are the signs of kidney failure in dogs?
- How will the vet diagnose kidney disease?
- What is the treatment for acute kidney failure?
- What is the treatment for chronic kidney disease in dogs?
- Is kidney failure in dogs painful?
- How can you comfort a dog with kidney failure?
- What is the prognosis for kidney failure in dogs?
- Lean on your veterinarian's wisdom
- 3 dogs and 3 different approaches to kidney failure
- Have you navigated kidney disease with your beloved dog?
What is kidney failure in dogs?
Kidney failure in dogs is the condition that occurs when the kidneys are not functioning at their normal capacity. But don’t let the word “failure” scare you. Understandably, when you hear the term kidney failure, your mind likely jumps to worst case scenarios and grave prognoses for your dog.
To those in the medical community, however, kidney failure doesn’t necessarily mean end-stage disease. Veterinarians often use the term “kidney failure in dogs” somewhat interchangeably with the term “kidney disease in dogs.”
You also may hear or see terms like “renal failure,” “renal disease,” or “renal insufficiency.” Without additional context, each of these terms alone doesn’t tell you much about how severe the problem might be. However, what they all have in common is that they are various ways to say that the kidneys aren’t working as well as they should.
Where are a dog’s kidneys? What do they do?
In veterinary school we had to learn anatomy and physiology before they would teach us the fun stuff (i.e. all the diseases and how to fix them). Though I didn’t love it at the time, I guess they did have a point.
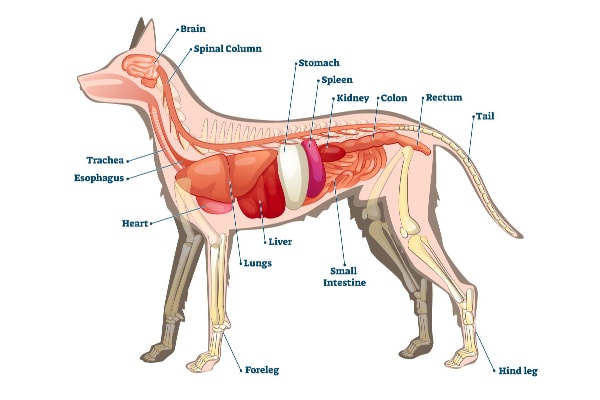
So, let’s start with a little anatomy and physiology lesson.
Dogs, just like people, have two kidneys, one on the right and one on the left. Your dog’s kidneys are in their upper abdomen tucked up under the ribs near their back.
If you have ever potty trained a puppy or rushed home to let your older pup out to potty, then you are all too familiar with the most well-known job of the kidneys—making urine. The urine that the kidneys make, however, is just a by-product of several lesser known but highly vital jobs performed by these powerhouse organs.
What do the kidneys do?
The kidneys are responsible for:
- Filtering toxic waste products from the blood
- Balancing levels of essential electrolytes
- Preserving hydration by conserving just the right amount of water
- Helping regulate calcium and phosphorus levels
- Controlling blood pressure
- Stimulating the bone marrow to produce new red blood cells
One of the more important points to note about the kidneys is that kidney cells can’t grow back or regenerate. Some other organs, like the liver, can regenerate after they are damaged. But when it comes to the kidneys, dogs aren’t going to get any more kidney function than they were born with.
To make up for this fact, the body builds in an impressive reserve capacity. Human kidneys are the same. This explains why you can donate one of your kidneys without experiencing any major long-term health issues or outward signs of decreased kidney function.
However, even with this reserve capacity, it is possible to reach a point where so many kidney cells are lost that the kidneys can no longer do their jobs. Now the dog is in kidney failure.
What are the types of kidney failure in dogs?
There are essentially two main types of kidney failure—acute and chronic. A third type, acute-on-chronic, is a bit of a mixture of the first two types. Acute-on-chronic is when a dog with chronic kidney disease that is stable experiences a sudden worsening of their kidney function.
Each type has different lists of potential causes, different focuses of treatment, and different prognoses. For this article, we will stick to acute and chronic kidney failure in dogs.
How fast does kidney failure in dogs happen?
In the case of acute kidney failure, the kidneys fail very rapidly—potentially in hours or days. But chronic kidney disease and renal failure can be slowly progressive over months or even years. Therefore, there isn’t really one set speed at which kidney failure in dogs occurs.
What causes acute kidney failure in dogs?
As the name implies, acute kidney failure comes on suddenly, usually in a matter of days. It is caused by a major injury to the kidney. There are certainly some well-known causes of acute renal failure, but frustratingly, it is not uncommon for veterinarians to be unable to pinpoint the exact cause of the kidney injury.
Some of the well-known causes of acute kidney failure in dogs include toxicities, medications, foods, infections, anything that decreases blood flowing through the kidneys, and anything that obstructs the flow of urine out of the body. I will dig into each of these causes in more detail below.
What toxins cause kidney failure in dogs?
There are several common household products, medications, or supplements that have the potential to cause acute kidney failure:
- Antifreeze (i.e. ethylene glycol)
- Cholecalciferol rat poison
- Dog eating grapes or raisins
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Aminoglycoside antibiotics
- Vitamin D
Let’s take a closer look at each of these toxins
Antifreeze
Antifreeze tastes sweet so it is enticing for dogs. However, even small amounts of ethylene glycol, the toxic agent in antifreeze, can be dangerous. When a dog drinks or licks up antifreeze, the body breaks the ethylene glycol down into several toxic substances which can directly and indirectly damage the kidneys.
Cholecalciferol rodenticide
While there are several types of mouse and rat poisons that are toxic to dogs, cholecalciferol-based rodenticides are the ones that target the kidneys. Among other problems, cholecalciferol (Vitamin D3) causes hyperphosphatemia (i.e. increased blood phosphorus) and hypercalcemia in dogs (i.e. increased blood calcium), which in turn can significantly damage the kidneys. The end result is acute kidney failure.
Grapes and raisins
Although the exact mechanism of toxicity is still under investigation, it is well established that eating grapes and raisins can cause acute kidney failure in some dogs. However, other dogs eat grapes and raisins their whole lives with no ill effects.

Non-steroidal anti-inflammatory drugs (NSAIDs)
Over the counter non-steroidal anti-inflammatory pain medications (NSAIDS) like ibuprofen (Motrin or Advil) and Naproxen (Aleve) may be great at relieving your aches and pains. However, you should not give your dog Advil or any of the other medications on that list. These medications, even at modest doses, can cause kidney failure in dogs.
Dog-safe NSAIDS like carprofen for dogs (Rimadyl®) are generally well-tolerated but can occasionally unexpectedly damage the kidneys, even at the correct dosage. This explains why your veterinarian might want to check bloodwork one to two weeks after starting these types of medications.
Also, many doggy NSAIDS are meat flavored. Severe kidney failure can result if a curious pup accidentally gains access to the entire bottle and ingests too many of the tempting tablets.
Aminoglycoside antibiotics
A certain class of antibiotics, aminoglycosides, have a higher potential to cause acute kidney injury when compared with other antibiotics. While this sounds scary, please know that your vet will weigh the risks and benefits carefully before prescribing aminoglycosides to treat bacterial infections.
Vitamin D
If a dog gets into a bottle of vitamin D supplements, licks Vitamin D-containing topical psoriasis medications off a person’s skin, or chews on the tube of psoriasis medication, he or she may develop hypercalcemia and kidney damage.
SAFTEY PSA: It is so important to store all medications and toxins safely away from your dog. Also, it is important to never give your dog any medications without talking to your veterinarian first. If you dog does eat or drink any of the items on this list, you should call a veterinarian immediately. In some cases, quick treatment can prevent severe kidney damage.
Infections
Infections can also cause acute renal failure, typically in one of two ways. The first is when a urinary tract infection (i.e. UTI in dogs) is left untreated. The bacteria can travel up from the bladder to the kidneys, where they set up shop and cause a kidney infection (i.e. pyelonephritis in dogs). The ensuing bacterial infection causes the affected dog to feel ill and can lead to kidney damage.
The second occurs when an infectious disease called Leptospirosis causes acute renal failure. Leptospirosis is caused by a bacteria that is spread in water contaminated by the urine of infected wild animals or rodents. Luckily, vaccines exist for many, but not all, of the strains of leptospirosis.
If you’re unsure which dog vaccines are necessary for your pooch, talk to your veterinarian. He or she can suggest a vaccination plan based on your dog’s age, lifestyle, and risk factors.
Decreased blood flow to the kidneys
Anything that causes decreased blood flow to the kidneys can lead to acute kidney failure. Low blood pressure deprives the kidneys of vital oxygen and nutrients. If that low blood pressure is sustained for long enough, the kidneys can incur permanent damage. Some specific causes of low blood pressure that might lead to acute renal failure are:
- Severe dehydration
- Sepsis
- Heat stroke in dogs
- Congestive heart failure in dogs as a result of heart disease in dogs
- General anesthesia

It is important to note that these conditions will not always lead to kidney failure. The thought of your dog going under general anesthesia can be nerve-wracking enough without having to worry about kidney failure, so I want to take a moment to specifically address this potential cause.
Anesthesia and kidney failure in dogs
Veterinarians generally take extra precautions to protect the blood flow to the kidneys during anesthesia. They do this by using the lowest possible doses of anesthetic medications and by giving IV fluids and monitoring blood pressure closely during anesthesia. The vast majority of dogs who undergo general anesthesia recover uneventfully.
So if you are wondering “Is my dog too old for anesthesia?” or “Is my dog too old for surgery?” don’t let the fear of kidney failure get in the way. Instead, have a conversation with your vet about it.
Urinary obstruction
Urinary blockages can also cause acute kidney failure because the kidneys continue to make urine even if a blockage is present. This urine backs up within the kidneys, which have a relatively inelastic outer membrane. The pressure from this buildup can lead to cell death.
The longer the blockage is present, the more permanent damage occurs. Blockages can be caused by kidney stones (i.e. nephroliths and ureteroliths), bladder stones (i.e. cystoliths), or tumors within the urinary tract.
What causes chronic kidney failure in dogs?
Based on the name, you can infer that chronic kidney failure refers to a much more gradual process where the kidney function declines slowly over a long period of time. Unfortunately, a specific cause tends to be more difficult to pin down than with acute kidney failure.
In some cases, the loss of kidney function is due solely to age-related degenerative changes. Basically, more and more kidney cells wear out over time, leading to decreased overall kidney function. In other cases, genetics, immune-mediated disease, or chronic non-kidney related illnesses (like high blood pressure or diabetes in dogs) can play a role in kidney problems.
Remember I mentioned earlier that every dog is born with extra kidney function? Well, this means that chronic kidney disease (CKD) can be present for quite a long time before any obvious signs of decreased kidney function become outwardly apparent.
What are the signs of kidney failure in dogs?
As the kidneys continue to fail, the dog will reach the point where he or she does begin to show some of the following symptoms of kidney failure:
- Increased thirst and increased urination (or decreased urination in severe acute kidney failure)
- Decreased energy
- Weakness
- Decreased appetite
- Weight loss
- Nausea
- Vomiting and diarrhea
- Hypersalivation
- Ulcers in the mouth
- Black tarry stools
- Bad breath
- Pale gums
- Blood in the urine
Let’s take a closer look at each of these symptoms.
Increased thirst and increased urination (or decreased urination in severe acute kidney failure)
Increased thirst in dogs and increased urination is often one of the first signs of chronic kidney disease. The kidneys help maintain hydration by making concentrated urine. With kidney disease, this concentrating ability is the first thing to go, leading to the production of copious volumes of dilute urine. To make up for all this urine, dogs with kidney disease must drink more water.

NOTE: In severe acute kidney failure in dogs, the kidneys might be damaged to the point that they are making very little urine (i.e. oliguria) or no urine at all (i.e. anuria). In this case, you would actually see decreased urination rather than increased urination.
Decreased energy
You might notice your dog laying around or sleeping more, not wanting to participate in normal daily activities, and just generally being a lethargic dog.
Weakness
It may seem like your dog is struggling a little more to get up and move about or do the things (e.g. jumping up on the couch) that he or she once did with ease. Sometimes your dog’s legs might tremble or he or she will need to lie down and rest frequently.
Decreased appetite
Especially as kidney failure progresses, the toxins that build up in the blood can make your dog feel sick and be less likely to want to eat. Your dog may turn up his or her nose at dog food but still eat treats, or he or she may not want to eat at all.
Weight loss
As time goes on, your dog might also start to lose weight. His or her bones may look more prominent or he or she may seem to have less muscle mass.
Nausea
The toxins that build up due to the kidney’s inability to remove waste products from the blood can make your dog feel very nauseous. You might notice your dog keeps licking his or her lips or is drooling excessively.
Vomiting and diarrhea
In addition to feeling nauseous, your dog might also start vomiting. Or he or she could have diarrhea too.
Hypersalivation
One of the indicators of nausea is increased salivation. Therefore, you might notice a dog with kidney failure starts drooling more than normal.
Ulcers in the mouth
In severe cases of kidney failure, the dog may develop ulcerations on the tongue or elsewhere in the mouth. These are known as uremic ulcers.
Black tarry stools (i.e. melena)
Sometimes you might notice your dog’s poop looks dark and sticky or has a coffee-ground appearance. This is an indicator of GI bleeding.
Bad breath
Dogs with severe kidney failure may develop a specific type of bad breath in dogs known as uremic breath. They may have an ammonia or urine smell to their breath. (This is not to be confused with the bad breath from dental disease in dogs.)
Pale gums
Because the kidneys play a vital role in stimulating red blood cell production, dogs with kidney failure may develop anemia in dogs (i.e. low red blood cell numbers). One of the main signs of anemia is pale gums.
Blood in the urine
If your dog has a concurrent urinary tract infection, (either as a cause of acute kidney failure or as a consequence of chronic kidney disease) you might notice bloody urine, straining to urinate, or increased frequency of urination. However, in a study of 201 dogs with chronic kidney disease, while 32% of them had evidence of a UTI on a urine culture, most were asymptomatic.
Signs can vary depending on the severity of the kidney failure
Early in chronic kidney failure, your dog might just have increased thirst or increased urination (or no symptoms at all). But with acute kidney failure, or with the later stages of chronic kidney disease, your dog is more likely to feel outwardly ill. He or she may experience any combination of the symptoms above.
If you think your dog might be showing signs of kidney failure, please make an appointment with your veterinarian promptly. Early diagnosis can help slow the progression of chronic kidney disease. And it is important to be able to start treatment as soon as possible for acute kidney disease.
How will the vet diagnose kidney disease?
If you or your veterinarian are concerned that your dog may have kidney disease, the first step is a complete physical exam and blood and urine tests.
Bloodwork
Your veterinarian will want to perform a chemistry panel, which includes the two main markers of kidney function, BUN and creatinine. That blood test for dogs can also check the levels of electrolytes like phosphorus and potassium. Sometimes those levels are altered in dogs with more significant kidney failure.
Urinalysis
To accurately interpret the BUN and creatinine levels, your veterinarian will also need a urine sample from your dog. It is important to note that the BUN and creatinine can be high in dogs who are dehydrated from non-kidney related illness. In these dogs, their urine will be concentrated, and their urine specific gravity will be high. On the other hand, a dog in kidney failure will have high BUN and creatinine levels with dilute urine.
Low urine specific gravity (i.e. very dilute urine) is actually the first indicator of chronic kidney failure. The urine becomes dilute before the BUN and creatinine levels rise.
Correlation between test results and kidney function
By the time the kidneys lose their concentrating ability, 66% of your dog’s kidney function has already been lost. This explains why it often seems like kidney disease has snuck up on you and your furry family member. BUN and creatinine levels finally begin to rise when more than three-fourths of your dog’s kidney function has been lost.
Put another way, by the time your veterinarian is able to pick up kidney disease with a standard blood panel, only 25% of your dog’s kidney function would remain. Your dog must lose even more kidney function before he or she would show outward signs of feeling sick from the elevated BUN and creatinine (i.e. waste products in the blood).
This explains why it is so important to consider yearly screening lab work for your senior dog and why this lab work should ideally also include a urinalysis. Knowledge is power in this case. Finding chronic kidney disease as soon as it becomes detectable on bloodwork and urinalysis means being able to take steps to slow its progression sooner.
Additional testing
If your vet has diagnosed your dog with kidney failure, he or she may also recommend additional testing such as:
- Blood pressure measurement—uncontrolled high blood pressure (i.e. hypertension in dogs) can worsen kidney failure.
- Urine culture—to check for evidence of a urinary tract infection.
- Abdominal ultrasound—to assess for masses or blockages within the urinary tract and/or look for visual changes to the kidneys that might suggest either an acute kidney injury or more chronic degenerative kidney disease.

Based on the results of the lab work, additional testing, and your dog’s history, the veterinarian will determine if your dog most likely has acute kidney failure, chronic kidney failure, or acute-on-chronic kidney disease, and start treatment accordingly.
What is the treatment for acute kidney failure?
Intravenous fluids are the main treatment for acute kidney failure. The elevated BUN and creatinine levels that tell your veterinarian that your dog is in kidney failure also make your dog feel sick. This is because BUN and creatinine are toxic waste products that the kidney normally eliminates. Ideally, IV fluids help flush out the kidneys and bring these levels down.
If you find yourself in this situation with your dear dog, it is best to expect an inpatient hospitalization with multiple days of IV fluids. Each day, your veterinarian will recheck your dog’s kidney values to see if they are improving. Once the improvement slows, your veterinarian will attempt to gradually wean your dog off IV fluids to see if the improvements persist.
If your dog is hospitalized for acute kidney failure, your veterinarian will likely consider adding in some other treatments in addition to the IV fluid therapy. He or she may often administer IV antibiotics in case the acute kidney failure could be due to pyelonephritis (i.e. kidney infection) or leptospirosis.
Most other treatments fall into the supportive care category and are aimed at helping dogs feel better during their stay. These might include anti-nausea medications (e.g. Cerenia for dogs), antacid medications (e.g. omeprazole for dogs), pain medications, and appetite stimulants for dogs.
Response to treatment
One of the most difficult parts of trying to counsel dog parents through this particular diagnosis is that it’s impossible to tell at the outset of treatment how a dog might respond. In some cases, the kidney values will slowly return to normal. In other cases, the values might initially improve but stabilize at a level that is still above the normal range.
And, unfortunately, some dogs do not improve despite appropriate and aggressive treatment. In those cases, dog parents and veterinarians face a difficult choice. Many decide that euthanasia, while heartbreaking, is the right choice to prevent their beloved dog from suffering.
While deciding when to euthanize a dog with kidney failure, some dog parents may take advantage of hospice care for dogs. This can help keep their dog comfortable while giving them time to prepare for their dog’s euthanasia.
Other dog parents in that situation may decide to pursue dialysis, which can allow extra time for the kidneys to recover from an acute injury. Dialysis requires intensive care and monitoring and is only available at certain veterinary specialists. The requisite intense level of care and lengthy hospitalization can make dialysis cost-prohibitive for many dog parents.

What is the treatment for chronic kidney disease in dogs?
While both types of kidney disease involve a loss of kidney function, veterinarians treat chronic kidney disease quite differently than acute kidney disease. Unfortunately, chronic kidney disease is incurable and progressive. No medication or treatment can stop the ongoing loss of kidney function.
The good news is that treatment can slow down the rate of progression in many dogs. The even better news is that a significant proportion of dogs with chronic kidney disease can have a good quality of life for many months to years with proper management and close monitoring.
Your veterinarian will tailor the treatment for chronic kidney disease to your individual dog. Official guidelines exist that lay out the stages of kidney disease in dogs. These same guidelines offer treatment recommendations unique to each stage.
Chronic kidney disease treatment may include:
Kidney diets for dogs
Prescription kidney-friendly diets are an important part of the management of chronic kidney disease. These diets have lower protein and phosphorus levels and put less strain on the kidneys.
Blood pressure medications
You veterinarian will also want to closely monitor your dog’s blood pressure. If your dog develops high blood pressure, your dog’s doctor will likely recommend oral blood pressure medications. We already talked about the fact that high blood pressure can contribute to chronic kidney disease.
But chronic kidney disease in dogs can also lead to the development of high blood pressure. Uncontrolled high blood pressure, in turn, can then hasten the loss of kidney function. And so the cycle continues.
Medications to manage proteinuria
Protein loss in the urine (i.e. proteinuria) is a similar chicken and egg phenomenon to high blood pressure causing kidney disease and kidney disease causing high blood pressure. Consequently, vets also try to monitor and address urine protein levels in dogs with chronic kidney disease.
As the kidneys degenerate, the filter portion (i.e. glomerulus) of the kidneys can become leaky. Proteins that the kidney should keep within the bloodstream are then able to leak out into the urine. So, protein in the urine is a sign of kidney disease in dogs, but that leakage of protein through the kidneys can also hasten kidney damage.
Your vet may prescribe oral medication like enalapril for dogs to help decrease this protein loss.
Potassium supplements
Some dogs with chronic kidney disease will have low potassium levels, which can make them feel weak and tired. Your vet can easily monitor your dog’s potassium levels with routine bloodwork. If levels are low, the vet may recommend oral potassium supplementation.
Red blood cell support
The kidneys make a hormone called erythropoietin that helps tell the bone marrow to make new red blood cells. In some cases, late-stage kidney disease can cause anemia in dogs due to decreased production of this hormone.
If your pup is in this situation, your veterinarian may discuss injections of a synthetic version of this hormone to try to improve the anemia. Depending on the severity of the anemia, your dog may also need a blood transfusion. This can be a way to boost red cell numbers while waiting to see if the synthetic hormone injection will work.
Subcutaneous fluids
Administering fluids under the skin (i.e. subcutaneous fluids for dogs) can be a great way to help dogs with later stage kidney disease stay hydrated and feel better for a longer period of time. This can help improve their quality of life. Plus, it can keep them out of the hospital so they may enjoy their time at home with their loving family.
The idea of giving your dog fluids might sound scary. However, many dogs tolerate having this done at home, even on a daily basis, surprisingly well. If your dog has late-stage kidney disease and would benefit from subcutaneous fluids, your veterinarian or veterinary nurse can show you exactly how to give the fluids. The veterinary team can also give you some tips to ensure you and your dear dog are as comfortable as possible with this process.

Is kidney failure in dogs painful?
While end-stage kidney disease is not necessarily painful, it can make affected dogs feel pretty icky. Your veterinarian will work with you to tailor a specific treatment plan to allow your dog to feel well for as long as possible.
As part of this treatment plan, your veterinarian might recommend medications to bind phosphorous in the intestinal tract, medication to help regulate calcium levels, anti-nausea medications, antacid medications, pain medications, or appetite stimulant medications. All of these can help manage the signs of kidney disease.
How can you comfort a dog with kidney failure?
In addition to giving your dog all recommended medications, there are also several other great ways to comfort a dog with kidney failure. First, a bit of TLC goes a long way. Sometimes just spending time with your dog or taking a few extra minutes to snuggle can really help him or her feel loved.
Plus, since kidney disease makes dogs urinate more and drink more, it is important to always have a bowl of fresh clean water easily accessible for your dog. And you should take him or her out for lots of potty trips so he or she can urinate when necessary. Should your dog have an accident in the house, clean it up without making a big deal out of it. Chances are your dog just couldn’t hold it any longer.
What is the prognosis for kidney failure in dogs?
As you have probably gathered from the different treatment options, the term “kidney failure” encompasses a wide range of situations—from a dog with non-symptomatic mild elevations in kidney values to the severely sick dog whose kidney values are off the chart.
Overall, the prognosis for acute kidney failure is somewhat guarded. Unfortunately, roughly 50% of dogs in this situation either die or are euthanized because of their condition. The response to treatment in the first few days can help determine how likely your dog is to recover. Your veterinarian can help counsel you through this challenging situation to determine the next best steps based on your dog’s unique situation.
For chronic kidney failure, the prognosis is highly variable and depends in large part on the stage of disease at the time of diagnosis. Dogs with early-stage kidney disease can live for years with stable disease and a good quality of life. On the other hand, dogs with late-stage renal failure may only feel well for a period of weeks or months.
Lean on your veterinarian’s wisdom
A diagnosis of kidney failure can be scary. Especially when you hear it is acute kidney failure or late-stage kidney disease, both of which tend to have a more bleak outlook. Being blindsided by a diagnosis of kidney disease after a routine senior dog physical exam isn’t easy either. All of these situations may leave you feeling worried and alone.
But you are not alone. Your veterinarian knows you and your pup well and is on your side. He or she will play an integral role in providing support and advice as you work together to give your dog the best life possible for as long as possible.
Granted, the treatment options are a bit more limited with acute kidney failure. But with chronic kidney failure, there are many ways to help keep your pup feeling good. In either situation, the best advice I can give is to take heart and talk with your veterinarian.
3 dogs and 3 different approaches to kidney failure
Before we wrap up, I’d like to share what prompted me to write this article. Recently, in the space of just a few days, I treated three dogs with kidney failure. Their names are Toby, Stella, and Oscar, and they were the inspiration for this article. Allow me to briefly share their stories.
Toby: A Dachshund who suffered from acute kidney failure
First there was Toby, a handsome older Dachshund. He had a bad bout of pancreatitis in dogs and became dehydrated. The combination of dehydration and pancreatitis led to acute kidney failure. Happily, Toby recovered after being hospitalized for five days.

Stella: A Toy Poodle with high kidney values
The very same day I discharged Toby, I saw Stella for her six-month check-up. Stella, a perfectly coiffed 12-year-old Toy Poodle, had borderline elevated kidney values last year. Though Stella was feeling great, her bloodwork from her visit that day revealed that her kidney values were higher than before. I called her parents and let them know it was time to switch her to a kidney-friendly diet.
Oscar: A Frenchie with a history of chronic kidney disease
Then, the very next day, I saw Oscar, a grey-muzzled Frenchie, for the first time, and was immediately smitten. Oscar had a history of chronic kidney disease that had been well-managed for years with a prescription diet. So elevated kidney values weren’t a surprise on his bloodwork. But Oscar’s testing that day revealed two new problems—protein in his urine and high blood pressure.
I am lucky to care for patients like Oscar (who is doing well on his new medications by the way), but I must admit that after his appointment I was ready for a few days respite from kidney issues.
I can take a hint though, and the universe was obviously trying to tell me something, so out of their stories, this article was born.
Have you navigated kidney disease with your beloved dog?
Please comment below.


My Kelsey had kidney disease . Unfortunately the vet’s information on it was NOT as thorough as what Ive just read . But he put her on meds and special diet. He said when it would hit her it would be bad and fast. Well it did. It was the middle of the night and she was having bloody and runny stool all night, all over herself. She was embarrassed I think because she couldn’t get up. And go to the bathroom outside. But I cleaned her each time and told her it was alright. My whole house smelled like blood and poop. From all the stuff coming out of her. We put blankets and padding under her and used puppy pads under her bottom to catch everything. She was a big dog and it was very cold out and I couldn’t get her in the vehicle because she was just having uncontrollable bowel . It was the worst night I’ve ever been through. My girl was dying and I couldn’t get her to the vet so they could help her along. We spent the whole night talking to her cleaning her up because she couldn’t get up. She was such a brave girl never cried or whimpered just layed there while I cleaned her up over and over. . My Kelsey passed early the next morning after going through hell all night . I’m crying typing this. I miss her and that was a terrible horrible night . I pray and talk to her still and ask God to take care of her for me … I miss her so much. ❤️🙏🐶🐾
Dear Kristie,
My heart aches for you with the recent loss of your beloved Kelsey. I am so sorry her last night was horrible but know that your presence was a comfort in those difficult hours. I am thankful you were able to be with her until the very end. I hope with time your heart can begin to heal and the memories of the good times will replace the grief. Wishing you brighter days ahead. Bless you. ♥
Pet Loss Support: Groups & Resources for Comfort
Hi everyone,
My 4-year-old Golden Retriever, Goldy, suddenly vomited 4 times in a day, so we rushed him to the vet.
Age: 4 (turning 5) Test Type: Biochemical Blood Report Date of Report: May 4 (the day of him vomitting 4x)
Results: • TP (Total Protein): 7.10 g/dL (Normal, range 5.4 – 8.2) • ALB (Albumin): 3.10 g/dL (Normal, range 2.5 – 4.4) • GLO (Globulin): 4.00 g/dL (Normal, range 2.3 – 5.2) • A/G (Albumin/Globulin ratio): 0.80 (Normal, range 0.5 – 2.0) • TBIL (Total Bilirubin): 0.32 mg/dL (Normal, range 0.1 – 0.6) • ALT: 54 U/L (Normal, range 10 – 118) • ALP: 27 U/L (Normal, range 20 – 150) • AMY (Amylase): 2061 U/L (High, range 200 – 1800) • CHOL (Cholesterol): 265 mg/dL (Normal, range 124 – 271) • GLU (Glucose): 72 mg/dL (Normal, range 59 – 110) • CRE (Creatinine): 7.79 mg/dL (Very High, range 0.3 – 1.3) • BUN (Urea): ≥100 mg/dL (Very High, range 7 – 25) • BUN/CRE Ratio: 15 • Ca (Calcium): 11.20 mg/dL (Normal, range 8.6 – 11.8) • P (Phosphorus): 8.78 mg/dL (High, range 2.9 – 6.6) • K+ (Potassium): 4.00 mmol/L (Normal, range 3.7 – 5.8) • Na+ (Sodium): 143 mmol/L (Normal, range 138 – 160) • Na+/K+ Ratio: 36 (Normal) • TBA (Total Bile Acids): 0.35 µmol/L (Normal, range 0 – 15)
He’s day 2 now on 5 days of IV fluid therapy, and the vet said if his levels don’t drop, He needs to take medications his whole life. But we’re also hoping this is a temporary spike from vomiting and dehydration (maybe acute-on-chronic injury?).
I’m staying positive, but I’m also scared. Goldy is still young, active, and full of life. We’re ready to give him full care — renal diet, fluids at home, meds, everything.
I have a few questions: Can he live a good life for another multiple to several years? What happens if his levels come down? • Has anyone had a dog whose kidney numbers improved after fluids? • If his creatinine drops to 3–5, is it possible for him to live more than 3-4 years with full care? • What kind of long-term care routines have worked best for your dog? • Any tips for stopping dogs from eating grass/leaves or sneaking food?
Any similar stories, guidance, or encouragement would mean a lot to me. Thank you.
Hi Vedant,
I am sorry Goldy is facing this unknown issue with his kidneys. I understand your concern and think he is very lucky to have you advocating for his health and well-being. Unfortunately, without knowing the cause of these elevated kidney values or if this is a chronic or acute problem, I can’t really make conclusions as to what Goldy’s prognosis will be. There are MANY dogs that have endured an acute kidney injury that were able to make a full recovery with the right treatment. Here is a link to another article with more information and great comments from other readers as well: Kidney Disease in Dogs: Stages and What They Mean For Your Dog
Hoping your sweet boy will begin to improve and praying for a positive outcome.
Hi. Just received the DX of Stage Three Kidney Failure for my appox 10 year old rescued Shih Tzu – my only child. I am also a retired RN so know the lab work pretty well. I was thinking Diabetes or Cushing’s or both but not renal disease. His BUN was 103 & creatinine was 2.2. However he has 2+ Protein in his urine as well as Trace occult blood. His sp. gravity in urine is still 1..017 which is WNL (within normal limits). Has anybody given IV fluids at home.? I have 40 years of hospital nursing but that doesn’t translate to dogs. I am a senior – 79 years old & could use a little advice as to what to expect for my Son who is my constant companion. I used to have Pugs but the shedding got to be too much & Jack came along as a rescue. He doesn’t shed. Thanks for listening.
Dear Jill,
I am sorry Jack has received this difficult diagnosis. While IV fluids are not routinely done at home, I have had many clients give subcutaneous fluids at home to dogs with renal failure. There are lots of treatment options and things that you can try to help slow the progression. Here is a link to another article with more information: Kidney Disease in Dogs: Stages and What They Mean For Your Dog
I encourage you to talk with your vet and discuss your concerns. They can let you know if medications are needed or advise you if your pup should be on a prescription diet. Wishing you all the best as you navigate this unknown path. Bless you and your sweet boy.
Hi Jill,
I was reading this article and saw your post about your 10 year old shih tzu. I’m praying your only child is still with you. I also have an only child who is a shih tzu. She’s 13, weighs 5.5 pounds and has kidney disease. Her BUN is 101, her Creatinine is 3.9 and her SDMA is 47. We are managing the best we can. As far as IV fluids go, I’ve had to give them to my baby girl for almost a year now. She went from getting fluids once a week to twice a week to every other day. It’s still tough but it’s what she needs. I always worry I’ll put the needle in wrong or hurt her. BUT, as you know, we would do anything for our babies. My thoughts and prayers go out to you. Kathy
Dear Kathy,
I am sorry for all your senior girl has been through, but she is very lucky to have you taking such good care of her. Thank you for reaching out to offer support and sympathy to others. Wishing you both all the best and praying for many happy days ahead for your sweet pup.
My Redbone Hound, MaeMobley, went to vet Nov 4 for a swelling between two toes. Allergy diagnosis.
Vet said gums looked pale. Ran bloodwork. Creatine level was 3.2
BUN was 44.
Switched food to chicken)rice.
Jan 2 levels had risen to
Creatine 9.4
BUN 81
No weight loss. (96 pounds)
She eats well. No excessive thirst or urination. No vomiting. No diahrea. Normal activity levels.
Repeat bloodwork scheduled for 1/22/25.
What could possibly cause such high numbers with no other symptons?
Anything?
Thanks for any ideas.
Hi Wendy,
I am sorry your girl is facing this unknown issue with her kidneys. I wish I could offer some advice but there are just too many possible causes for something like this. Many times, dogs don’t show symptoms until the disease is very advanced. To get answers it may take more in-depth testing such as abdominal ultrasound, urinalysis, or even a consultation with a specialist. Hoping you can find a way to get the kidneys functioning as best they can. Praying for healing and a positive outcome for your sweet MaeMobley.
We are in the midst of kidney disease diagnosis as we are having a normally well trained dog urinating on the floor and drinking a lot. His levels have gotten worse over the past two weeks, but he seems energetic, eating fine, normal except for the numbers. He doesn’t have a UTI, leptospirosis, stones. He doesn’t seem to be urinating or drinking more than two weeks ago, but I guess his levels have gotten worse.
Dear Sandra,
I am so sorry you are facing this difficult diagnosis in your beloved pup. I am hoping with some diet changes and treatment your vet can get things to stabilize. How are things today? Praying for healing and wishing your sweet boy all the best.
My beloved Chiweenie Pasta was diagnosed with Kidney failure. She has lost so much weight and we have switched her to a Prescription Renal diet. I have a question – any idea on why she keeps licking the floor? She never did this before but she cannot help herself – she will just roam around like a roomba licking the floor. Anyone else experience this?
Hi Catrina,
I am sorry Pasta has been diagnosed with kidney failure. She is lucky to have you taking such good care of her and advocating for her health and well-being. I don’t think I have ever heard of that specific behavioral issue before and would not know how to link it to the kidney dysfunction. I wonder if she could possibly be experiencing early stages of dementia/cognitive dysfunction as well? Here is a link to another article with more information: Signs of Dementia in Dogs: Stages, Symptoms & Treatment
Hoping your girl will continue to maintain her quality of life for as long as possible. Wishing you both nothing but the best!
My 18 year old Jack Russell with stage 3 kidney disease was licking the floor too. She seems to have stopped doing it now – though she is also showing signs now of deterioration, uncoordinated and stumbling occasionally over the last 2-3 days. She’s still eating and moving about.
Dear Amanda,
I am sorry your senior pup is experiencing these worrisome symptoms. Hoping you can partner with your vet to offer her relief and ensure she maintains her quality of life for as long as possible. Wishing you both comfort and peace as you navigate this difficult path.
My jackobee turned 19 years old in may vet told me her kidneys are not filtering good now she is losing control of her backend but he told me she had a dislocation in the hind leg not sure why he didn’t want to treat it he put her on a probiotic and help her really well.. Now things are going down hill i can’t take it I love her so much. She will not let me love on her makes me sad..but I did want to say she has licked the floor but not as much as she used to
Dear Zanne,
My heart aches for you as you face this difficult situation with your pup. Hoping you can continue to find ways to keep her comfortable and wishing you both peace. ♥
Hi, I was just reading this article after hearing my 14yr old chihuahua has 75% kidney failure. Main symptoms are an increase in drinking water and urination plus blood found in urine. I wanted to respond because he is the second chihuahua I’ve had that obsessively licks floors. I’ve often wondered what the cause is and it made me smile to hear there’s others out there. All the best – Lisa and Mars
Hi Lisa,
How strange! You are now the 3rd person to say their dog licks the floor and was diagnosed with kidney failure. I am starting to wonder if there is in fact a connection between the two! Praying for Mars and wishing you all the best.
Hi everyone. My greyhound has also been diagnosed with kidney failure, at the age of 13, and is also licking the floor! Something she’s never done before. Very peculiar!
My wire hair doxie, 16, has kidney disease and has been on special diet for over a year. She gets utis frequently but this time it’s been more problematic. She was having blood in her urine and it was tested and was positive for bacteria. She went on an antibiotic and the blood stopped and then a couple days before her last pill blood appeared again. Vet put her on more antibiotics and it went away until a couple days before the last pill. We are scheduled for an ultrasound and culture but they only had availability in ten days. In the meantime is there anything I can do for her? She continues to have blood present, sometimes what looks like clots, frequent little puddles. What can I do for her in this in between time?
Thank you!
Hi Stephanie,
I am sorry your Dachshund is dealing with chronic UTIs. I understand your concern for her well-being and think she is lucky to have you advocating for her. Unfortunately, I am not aware of anything over the counter that will help with the symptoms. Some people have had good results with cranberry supplements for dogs but not all vets have them on the shelf. How are things today? Hoping you were able to get the urine sample sent off for the culture. Did you find out any new information after the ultrasound was performed? Feel free to leave an update if you have a chance. Wishing your sweet girl all the best and praying for complete resolution.
would probiotic help a dog with beginning of kidney disease?
Hi Tina,
This is a great question. I think probiotics are great and gut health can affect every organ system in the body. I am not sure how much of a benefit you will see with your dog’s kidney function, but adding in a probiotic certainly wouldn’t hurt. Best wishes to you and your pup!
i can’t thank you enough for writing this guide – all the info in one place, and from a reliable source !
our little spud just got hit with kidney problems, at 15, it all came on so suddenly. so i wanted to say how grateful i am to have found this article and your blog.
Hi Daisy,
Thank you for the kind words and positive feedback about the article. I hope your little guy will be able to keep fighting and I wish you both many happy days ahead. Bless you!
My question is if BUN and creatinine are normal but urine is diluted what’s the next step to find out if this is kidney disease . My vet mention about the diluted urine but he didn’t suggest anything else to do. I’m concern
Hi Alejandra,
I just responded to your other comment that was submitted on another article. I hope you will see it too. If I am concerned about early stages of kidney disease, I like to check an SDMA level on blood work. The SDMA will start to increase way before you will notice any changes with BUN or Creatinine. If all kidney levels are normal, then I am not sure you truly have a kidney problem. You can also talk to your vet about abdominal ultrasound, x-rays, or even a consultation with a specialist. Hoping you can find the answers you need to put your mind at ease. Bless you.
I am so thankful thank you for this article. I totally understand CKD in my little girl, Lola. She is 14yrs and was recently diagnosed with CKD and all her blood work was off the chart, per our doctor. I was totally devastated by this news. To make a long story short, we ended up putting her on IV fluids and she is responding better than expected. She is stage four and had lost so much weight, but now three months later she has gained one pound and seems to be doing well. Yes, she has her good and bad days. So we just take it day by day. I feel so fortunate that she still has her appetite and has been eating on her own. I also heard that they may have 14 to 80 days, so far she has been doing so much. You are, so much appreciated.
Thank you
Hi Louise,
I am sorry Lola is facing this difficult diagnosis but what a blessing she seems to be maintaining well for now. Thank you for the kind words and great feedback about the article. Praying for continued success and strength as you walk this tough road. Bless you and your sweet girl. ♥
Having navigated trouhought many different diseases with my rescues, I take them in as seniors and generally, they tend to not have had the most extensive veterinary care. My current dog, the love of my life, just turned 13. When I adopted him, his first bloodwork indicated high values (protein, UPC ratio). He was rapidly started on the “basics”, and put on a strict renal diet. He did not look ill, and has crazy energy for an old boy! He is a husky mix, and truly has a magic personnality.
Despite many behavioural challenges (trauma from being in a shelter), we found ways to provide good veterinary care (thanks to my dear Fear-free vet, to whom I owe everything!). I always had a very hard time doing research, but I’m so glad I finally found your page. From what I read online, the numbers surrounding life expectancy were very scary, and I would have never thought that 2 years later, he would be doing so well. He had X-rays, ultrasounds, his medications have been adjusted over the years, and so far, he has supported them very well.
I’ve had the amazing chance to see him grow into an even more confident boy, having a senior rescue is truly a special experience. Enjoying things of life, learning what he likes and doesn’t like.
Over the years, I have found it very hard to see vulnerable people like me, who love their pets so much, have to experience chronic kidney disease. I can proudly say that I not only admire veterinarians, technicians and everyone who helps me to help Whisky, I am forever grateful. You guys are heroes, you do a terrific job and might not always get the recognition you deserve. I hope my small commentary gives hope and/or puts a smile on someone’s face.
I wish I could show you a picture of what he looks like now, far from the frail old boy with a terrified look in his eyes I met on a freezing evening in November 2021.
Hi Juliette,
You are such an angel to be willing to take in senior dogs and give them a loving place to live out their final years. I appreciate the kind words and positive feedback about the article. Thank you for sharing your story and allowing us to learn about Whisky. Feel free to share his picture on our Facebook page! Wishing you continued success and happiness as you walk the path of life. Bless you and keep up the good work!
My 14 yr old Boston Terrier, Louie was diagnosed with Kidney Disease 3 weeks ago after a routine exam, since then, it’s almost like he heard the news and understood it better than I did, he stopped eating, developed pancreatitis and has been on a downward spiral ever since, we have him on an anti nausea, food stimulant and bp medication along with a prescription diet and antacid now, nothing seems to be working, his numbers weren’t alarmingly high, nor was his blood pressure so we definitely did not see this being so progressive 3 weeks ago, he goes back in to have his labs re-evaluated and hopefully the pancreatitis has passed but at this point we are feeding him through a syringe because he has refused any and all foods, even his favorites. I’m wondering if maybe a stay in the hospital with iv fluids may help?
Dear Renee,
My heart aches for you as you face this difficult situation with Louie. I too am shocked at how quickly things progressed but am glad your vet is monitoring him closely and acting quickly with treatment. You are correct that more intensive fluid therapy may be needed to help get things turned around. Don’t be afraid to speak up and advocate for your boy if you have ideas about treatment or any lingering concerns. Wishing you all the best as you navigate this unknown path. Bless you and your senior boy.
Just keeping you and you’re baby in my prayers. Hopefully you can find something that gets Louie back to some of his old self. After all, 14 is too early for him to leave you.
I, too, just got the bad news this week about my 22 year old beagle/Boston mix. His levels have significantly declined in the last 5 months. Due to his age and his many years of an enlarged heart and murmur, treatment is not an option. The only thing he will eat is chicken and broth and sometimes a small beef flavored treat. I know the protein is the last thing he should have, but he’s in his final days and I just pray he goes quietly in his sleep because I know he’s ready.
Dear Chris,
I am sorry your senior guy is nearing his final days. What a blessing you have shared 22 wonderful years together! Thank you for offering support to others as they navigate this difficult path. Wishing you and your sweet boy comfort and peace. Bless you both. ♥
Our 14 year old wire haired Dixie has chronic kidney disease with a couple numbers just over the normal range. He won’t eat the medicated food and now after 2 weeks of us giving him subcutaneous fluids he will not stand for it.. at all. Is there an alternative for us to get him his fluids? Are their meds? Should we take him to the vet every day to get fluids? Any info will be greatly appreciated. Thanks, Arnie
Hi Arnie,
I am sorry your senior guy is dealing with this difficult condition. While subcutaneous fluids can be very beneficial for dogs with later stage kidney failure, I am not used to recommending them when the kidney values on lab work are only slightly elevated. If this kidney dysfunction is a new development, it may be a good idea to ask about hospitalizing your boy for a day or two to allow for IV fluids which are much more effective in helping to flush out the kidneys. And yes, there are medications that can improve kidney function and allow for a better quality of life. Here is a link to another article with more advice on how to approach each stage of kidney failure and how to determine what stage your pup is in: Kidney Disease in Dogs: Stages and What They Mean For Your Dog
I encourage you to reach out to your vet and let them know the current treatment plan isn’t working well for you. Hoping you can find the best way to maintain your dog’s health for as long as possible.
My dog Bear has such a complicated blood work result. In October he had abdominal surgery for swallowing a piece of another dog’s toy.
Since the surgery, a new ‘symptom’ appeared as he began drinking a lot more water and having urinary accidents. Previous to the surgery, he had a ravenous appetite, and the Pica issue, and he does have a sort of pot belly (has for years). Suggested he may have Cushings.
However, also present in his recent bloodwork showed his kidney values were elevated (I think I’m saying that correctly). So that also could be, it seems from reading, the reason for his increased thirst/urination.
He also has pancreatitis – and the bloodwork was done during another ‘acute’ episode of pancreatitis.
My bigger wondering is: Could something in the surgery have caused his kidney function to be off? Damage? Meds? Anesthesia?
I will be scheduling Cushings testing, but it’s all so confusing. 6 months ago, I had a healthy dog (other than the pancreatitis that I controlled quite well with diet), and now I have a dog that is wearing diaper wraps, poor sweet Bear.
Hi Kat,
I am sorry Bear is facing this difficult situation and the last 6 months have revealed so many new issues. There is really no way to know why these kidney problems have surfaced. Kidney failure can develop very rapidly with little to no warning. It is possible for anesthesia to have an effect on kidney function but should not cause any issues unless there was already underlying kidney dysfunction prior to surgery. Even if you had known there was a previous kidney problem, I don’t see how surgery/anesthesia could have been avoided under these circumstances. For now, you are doing the right thing by moving forward with Cushing’s testing and focusing on treating the issues at hand. Praying for healing and relief for your sweet boy. Wishing Bear all the best.
Hi, my beloved little dog Daisy (10 year old Jack Russel-Beagle mixture) was recently diagnosed with chronic kidney failure. The vet recommended IV fluids & leaving her in the hospital for 2-4 days. This is all very new to me and I wanted to ask questions about this entire ordeal & the success rates of IV fluid treatment? How often would we need to bring her in for IV treatment following the first several days?
Hi Gaby,
I understand why you are worried about Daisy and wish I had some definite answers. Unfortunately, kidney failure is tricky and can be a bit unpredictable. IV fluids are used to try and help improve kidney function temporarily. It’s like a Band-Aid to restore some quality of life and offer more time. There is no way to know how much time this will give your sweet girl or if it will help at all. And follow up fluid treatments are based on how your girl responds and what her blood work rechecks show. This is one of those “wait and see how things go” situations. Hoping Daisy’s kidneys will respond favorably to the treatment. Praying for your comfort and strength as you navigate this difficult path. Bless you both. ♥
We are going through this now with our sweet girl Riley. She is an 8 year old Yorkie. We noticed her becoming lethargic last week not wanting to eat and an increase in thirst. We took her to the vet where she had extremely elevated white blood count. They administered fluids under the skin and prescribed antibiotics. Two days later we took her back to the vet due to no change. They again administered fluids under the skin and said continue with the medication. Two days later we noticed blood in her stool and took her to a different vet. They ran her labs and the numbers hadn’t changed from the first lab. They said she would benefit from IV therapy. She has been hospitalized on fluids today makes 5 days. We will go today to run labs and see if her count has changed. She seems perky and alert. She still hasn’t eaten (we are hoping this is just because of us not being there, she usually won’t eat unless we’re at home with her).
We will find out more today and hoping for the best!
Dear Amanda,
My heart goes out to you as you navigate this difficult path with Riley. Hoping her lab work will show some improvement and the treatment will help get things back on track. Praying for healing and wishing your girl the best. Feel free to leave an update if you have a chance.
I just lost my dog to what I believe is kidney failure. On Thursday my dog seemed absolutely fine – went for a walk, ate. played, drank. Friday Morning (7am), she went up my garden to do her usual business but by midday when i called her for her lunch she didn’t come. Then came the vomiting foam like substance and diarrhea, I called my vet ASAP who got us in for late afternoon. By that point, she had then gone off her legs. The vet didn’t seem overly concerned and thought it may be some sort of infection and gave antibiotics and a shot of painkillers. I had also mentioned that in the weeks leading upto this i had noticed increased thirst and increased urination as well as issues with her standing up when she got up from a sitting position. He said to come back Monday if no improvement and they would run bloods. Unfortunately just 48h later she had gone. I am still in disbelief that my dog who seemed like a healthy dog was fine one day and two days later gone. Is there anyway to tell if this was chronic kidney disease or acute kidney disease as it all happened so fast? The only tell tale signs (increased urination, thirst, trouble standing) only appeared just weeks earlier, is that more consistent with stage 4 chronic kidney disease? The worst for me is I don’t have any answers because there was no time to even get the bloods done. I would appreciate some insight as to whether chronic kidney disease which is advanced and undiagnosed could result in rapid deterioration so fast?
Dear Stephen,
My heart aches for you with the tragic loss of your girl. I understand how the grief can be overwhelming especially when you are left with more questions than answers. It is possible for kidney disease to progress rapidly and lead to death with little to no advanced warning. With that being said, you will probably never know for sure what contributed to the passing of your sweet girl. Try not to dwell on all the “what ifs” and instead find comfort in knowing she lived a good life filled with happiness and joy. May her memory live on and continue to be a blessing in your life. ♥
Thank you for your article it’s very informative!
Our English Bulldog is going through high kidney levels currently. He was diagnosed with 1 under developed kidney about 5 years ago so his levels were a stable 210ish.
Over the last week he stopped eating completely (not like him at all) and had very bad diarrhoea. He was still drinking but just really not himself! Admitted to the vets 72hrs ago with levels coming back at 670 and 42 so immediately put on fluids pain killers etc. There are signs of pancreatitis so they’re going to do detailed bloods on that today.
We are trying to remain positive as his levels have reduced to 470 and 32 so are hoping today’s results will be positive and lower.
I have read a lot about pancreatitis and he is showing all symptoms of chronic/ acute disease. The vet is convinced it’s his kidneys that are causing the symptoms but we want to be sure the pancreatitis isn’t effecting before making any permanent decisions and letting him go.
We just want to know we’re doing the right thing!
Sam
Dear Sam,
My heart goes out to you as you face this difficult situation with your Bulldog. I am hoping the intensive treatment was able to get him stabilized and the testing provided a clear path forward. How are things today? Praying all is well and your boy is back to living his best life. Feel free to reach out with an update if you have a chance.
I was told 3.5 years ago that my sweet boy had 3 months to live. He had stage 1 liver disease, polycystic kidney disease and pemphigus foliaceus. I could not accept that diagnosis. He was 12 at the time. I researched exhaustively and came up with an incredible regime that saw him return to his vital self for the most part. He is almost 16…one month to go. He is experiencing high urea and creatinine levels and i can see he is unwell. I am ramping up the regime and in addition to what I have given him in the past, I’m also adding activated charcoal. Studies look very promising for lowering creatinine and urea levels. I’ve started him on these today. I am also giving him quercitin that has a beneficial impact on kidneys. I hope my discoveries can help someone on this forum. I highly recommend 5 leaf bontanicals. Their herbs brought my very sick boy back to life. Good luck everyone. Never give up and do your own research!
Hi Di,
I am glad you were able to find what works best for your boy. What a blessing you have gained so much extra time together. Hoping the new therapies you are trying will show favorable results. Thank you for sharing your experience with us. Good luck and take care!
Thank you for giving such detail while explaining the different types of Kidney Disease.
My pup, Brownie was recently diagnosed with Kidney Disease. We took her in for some pre op bloodwork for dental cleaning. Sadly found out she was stage 2. Changed her diet and for about two weeks she was good. She loves her food and still reminded us to feed her and give her treats. A few days before her dental work she stopped eating her frozen blueberries. I truly believed it was because she had some sore teeth. She went in for her dental work and one tooth fell out on its own. Her doctor started her on fluids 2 hours before and left her on them for 2 hours after. She came home and was exhausted. That’s general anesthesia, right? So we let her relax. The next day, still not normal. By the end of the week she wouldn’t eat. This dog eats, so her not eating was worrisome. Heck, her not notifying me with barks to eat was worrisome. We started her in a low fat diet with thoughts that it was a pancreatitis flair up. 7 days after dental and she still wouldn’t eat. I went to our vet and demanded bloodwork. I needed to know what was going on. She was lethargic, refusing to eat, barely drinking but still hydrated. A day later the vet called. The dreaded news. My Brown girls levels tripled! In three weeks time and general anesthesia they tripled!! How was this possible?! Her Creatinine – 8.4, BUN – 202, Phosphorus – 22.6, SDMA – 68.
I was told to give her the best fighting chance I needed to get her to the ER Clinic in my area immediately. Today is day 4. Her numbers are slowly coming down. While visiting today she was starting to show signs of herself again. Still tired, but wagged her tail and was able to hold her head up. She even peed for us!
She is fighting her little dachshund heart out. With how fast this happened we believe it is acute on chronic and that she will be home soon. We know it takes time and as long as she has a fighting chance and is willing to fight we will support her.
This is such a terrifying time in our life but reading this blog post really helped me. Thank you again 🩵
Dear Brittany,
I am so sorry your little pup went through this terrible ordeal. What a blessing the veterinary team was able to work together to start the aggressive therapy needed to give your girl a fighting chance. How did things turn out? Hoping she was able to make a full recovery and all is well. Sending my best to you and yours. ♥
My 12-year-old English Springer has been diagnosed with chronic kidney failure. She is now on twice-weekly 400ml sQ fluids (handled by my vet’s technicians – it’s fairly cheap and I don’t want to take a chance of messing up the treatment at home).
My dog’s appetite is fine – she loves her food – but she is drinking more and more. She is lethargic, but I see that as a result of both her age and her chronic kidney disease. I’ve seen other comments here about naming the “stage” of her kidney failure. While I am familiar with stages of cancer, I don’t know what that means in terms of kidney failure.
I want to thank you for an easy-to-understand, well-written explanation of kidney failure in dogs. You have helped me understand and prepare for the inevitable, sad end.
Hi Chris,
So sorry to hear that your dog was recently diagnosed with kidney failure. Your questions about stages is a great one because knowing your dog’s kidney disease stage can help predict the prognosis and guide the treatment plan. I’ve included a link below to my article on the various stages of kidney disease. Determining her exact stage does require knowing the Creatinine and SDMA, so you may need to ask your vet for those numbers at the next SQ fluid visit.
I’m so happy to hear that this article was helpful, and I hope that the article on the various kidney disease stages will be helpful too. While you hopefully won’t need it for a long time yet, I’m also including a link to an article about when to euthanize your dog with kidney failure. It was written by an amazing end-of-life veterinarian and does a great job of discussing this difficult topic.
Here are those links:
1) Kidney Disease in Dogs: Stages and What They Mean For Your Dog
2) Dog Kidney Failure: When to Euthanize Your Dear Dog
My son and wife’s dog was taken for a follow up appointment at their vet for their dog’s eyes as they were bloodshot. They were worried it was Lepto so they sent them to a vet ER. He was tested negative. He started to get lethargic with a loss of appetite. After many visits to the vet, his kidney levels are high. He was given antibiotics but it isn’t helping. The vet got him on an antibiotic directed at the kidneys, but his kidney levels aren’t going down. The vet can’t find the exact reason for this, or what’s causing it. He’s taking appetite medicine to get him to eat. He did eat a bit last night. But this morning he was lethargic again and his back legs seem weak. The vet was told by the ER that the urine culture they took didn’t grow anything. He may be put on dialysis tomorrow for a couple of treatments. He’s not even 2 yet. He was a very healthy boy before all this. I now wish it was Lepto, so at least we would know what we’re fighting. This is so frustrating not knowing what is causing all this. So sad….
Hi Cathy,
My heart goes out to you, and to your son and his wife. I definitely understand that feeling of wishing it was Lepto because at least then you would know the cause and what to do for treatment. Not knowing can be so hard, and it can leave you feeling powerless. I’m sure the veterinary team feels much the same way. I hope that he starts to turn around soon and is able to have more good time with his family. Thinking about all of you! ❤️
Our 8-year-old English Setter was diagnosed with kidney disease about 9 months ago. It was actually found on some labs that she had as she has been on cyclosporine and ketoconazole for granulomatous blepharitis and my vet was keeping an eye on her liver functions. She has been placed on blood pressure meds, a prescription diet, which she doesn’t love, but I’ve tried adding things like chicken broth to the food to help her find it more appetizing. Some days she will hardly touch it and some days she eats it right up. She has never really exhibited any signs of kidney disease, and we probably wouldn’t have even known if the vet had not checked her BUN and creatinine levels. We have noticed that her breath smells terrible, and that is about the only thing noticeable besides her occasional appetite loss. So yesterday we took her to the vet for a recheck on her lab values. Her BUN and creatinine have ever so slightly increased. The vet says she is at a later stage 3. It’s a hard pill to swallow since she really doesn’t exhibit most of the symptoms of a dog in her stage of kidney failure. Our vet recommended subcutaneous fluids, and we started those yesterday. I know there is no way to stop the kidneys from getting worse, but I am praying that the medications she is on, the prescription diet, the subcutaneous fluids, and close monitoring by our vet is going to help us keep her going for as long as possible. It is breaking my heart to know that someday, probably a lot sooner than I want to think, that we are going to have to say goodbye to our sweet girl. We are going to fight with all our might to keep her feeling well and happy as long as we can. I am so, so appreciative of all the information I have found on this page. I read some of the heartbreaking stories of other dog parents with tears in my eyes because I feel their pain and I know I will be going through it too soon. Thank you for all the information and support.
Dear Kim,
My heart goes out to you as you face this difficult path with your senior girl. I hope the treatment can prolong her life and give you some extra quality time together. Just know you are not alone, and I am keeping you in my thoughts. Praying your sweet girl is surrounded by comfort and love and these last days are peaceful. ♥
My beloved, almost 13-year-old King Charles Cavalier, Lucy, stopped eating over the course of a few days at the beginning of March. This was very unusual for her, as she loved to eat. She’s diabetic and receives insulin shots twice a day so it was crucial she eat before her shots. We thought maybe it was her food and tried to change, but she refused it, and even her occasional favorites (boiled chicken, rice, etc.) she refused. I thought maybe it was a gastro issue. We took her to her vet right away, and he did a full blood workup (plus), 2 X-rays (one high-res), and a urinalysis. She has had a heart murmur since she was born, but it never posed a problem, and she has never needed medication for it. The vet was suspecting possible Addison’s disease due to her symptoms (lethargy, no appetite, weight loss, diarrhea but no vomiting), and he was hopeful we could treat that. We needed to wait overnight for the blood work to come back. As for prior illness, Lucy had a history of recurring UTIs that started about 4 years ago and was on antibiotics each time. We discovered the diabetes about 2 years later, after her glucose was through the roof (it had never been prior to that). My vet advised we go one step further and have an ultrasound done of her bladder to check for cancer (which was negative); she was tested for Cushing’s disease (also negative); and she was placed on Ursodiol for her gallbladder, which improved significantly with frequent checkups. She seemed to be doing well (besides slowing down with her age, diabetes, etc.). The day after her blood work came back, my vet called to say her creatine levels and BUN were so elevated that her kidneys were definitely failing and it was chronic (stage 4). He also said her liver was inflamed, there was protein in her urine, and the glucose level in her urine was very high. He did not think it was Addison’s because of how high her creatine/BUN numbers were. He suggested putting her in a 24-hour ER-type vet hospital with an IV, but thought it would be far too much strain on her heart and worried that she would go into congestive heart failure. She also was very anxious whenever she was away from home and we thought that would lead to more stress on her. We started treating her at home with IV fluids twice a day, using Azodyl (2 in the AM and 1 in the PM), and feeding her via syringe with special food. She was still moving and drinking but getting slower as the days went on. She would only eat via the syringe which she wasn’t crazy about and refused any hand feeding. She began vomiting (once a day, but this was unusual for her when she was healthy). She had ups and downs and seemed more agitated at night, so I would sleep right next to her. Unfortunately, about 10 days later, she declined significantly. She was very weak; she stopped eating and drinking, and her breathing became labored. We had to put her down that morning. It was the most devastating experience for myself and my family. As the days went by, my heart was so broken, I started to feel terrible guilt. I trust her vet and like him and he was always quick to recommend something when she was ill (which worked). He said the damage to her kidneys was so great there was nothing that could reverse it. However, I feel I should have gotten a second opinion or even tried the 24-hour ER fluids. If it was Addison’s disease, it could have been treated. I know it’s too late and there is nothing I can do to bring her back, but the guilt and regret I have are overwhelming. I can’t help but think I could have given her another chance or even a year or two of life. I was always faithful with her annual visits, and whenever I saw a potential illness or symptom that I thought would hinder her health, I had her checked. Having the kidney disease show up so suddenly and never an issue in the past was a shock. I’m having a tough time getting over it especially since she failed and died so quickly after her diagnosis. I miss her so much that my heart actually aches. I feel like I failed her and my children, who adored her as well. She was the best girl and my first and only dog. I don’t know if second opinions are common but if there is ever any doubt I recommend doing it.
Dear Liz,
I am so sorry for your tragic loss of Lucy. I know your heart is hurting and it is normal to ponder all the “what ifs” while grieving. From what you describe, it sounds like you made the right choice to offer your sweet girl freedom from her suffering. Your vet did exactly what I would have done in the same situation, and I honestly don’t think Addison’s was contributing to your pup’s condition. I always encourage second opinions if there are lingering questions or concerns. And I am fairly certain if you had pursued a second opinion you would have gotten the same diagnosis and prognosis. Please don’t hold onto the unnecessary burden of guilt over how things progressed. You did not fail Lucy and did everything you could to give her the best chance of recovery. I hope with time you will allow yourself some grace and be comforted knowing your girl was well loved. May Lucy’s memory live on and be a blessing to you and your children.
Hi, I’m sorry for your loss. I too just suddenly found out about my 14 year old Boo kidney failure. No wonder it’s called a silent killer, because you don’t know, until it’s too late. My baby’s outlook is grim. I will probably try treating him at home as well. I think that the best what we can do in such a situation is to give them our love and attention. Don’t blame yourself. I think you did your best to help her. I’m sure, she loved all your attention and the fact that she spent her last days at home, instead of being hooked up to some machines.
Dear Kate,
I am so sorry Boo has received this difficult diagnosis. Praying he can remain happy and comfortable for the time he has left. Bless you both and give your sweet boy a hug for me. ♥
My dog went dow to not eating or drink in 2 weeks. I’m homeless and without huge money to pay out, he’s 12
I’ve read your info and over and it helped me a lot . Your dog loved you
Dear Sinthia,
My thoughts and prayers are with you as you face this difficult situation with your pup. Please know you are not alone and feel free to reach out any time. Bless you and your sweet boy.
going through same rn with 12 yr old pit but she has stage 3. Diagnosed in late June. Started fluids 2x week and nausea meds she got alot better and been taking one day at a time. It’s hard and I feel your pain truly(this is my second dog that’s lived long life but it’s still so tough to say goodbye and watch them fade away) my advice don’t beat yourself up you did all u could do and if possible get new puppy asap. After my first dog died after bout with diabetes I was devastated especially since I was single then and without kid. She was my whole life but I got new puppy month or 2 after and it healed my heart but now I’m bk at that same situation with that puppy. Not alone anymore with gf and 4 yr old boy but it’s still hurting me badly.
Dear Collin,
I am sorry you are in this situation again with your senior girl. What a blessing she was able to heal your heart so many years ago and be by your side for 12 years. I know you will make sure she is happy and comfortable for all the days she has left. Wishing you strength to continue this journey. Bless you both.
I just lost my fur baby days ago. 3/31/2023 because my vet never really explained to me the side effects and potential deadly outcome of the long term use of carprofen. I was told “twice daily for pain.” and that it was like advil. they gave my a full jar, like it was safe.
6 weeks is all it took to destroy my Cloud’s kidneys. i noticed he was unable to go poop. so I added yougurt thinking he just needed something to help it along. I had no idea. The day we had him put down, his gums had turned white at the same time his kidneys were failing him. I’m so sad, if I only knew, my fur baby might still be with me.
The immense guilt I now feel. if I knew carprofen was going to do this, I would have researched alternative pain relief options for an injury that kept getting inflamed.
Dear Carolyn,
I am so sorry for your recent loss of Cloud. It is a tragedy this freak accident happened to your sweet boy. While there is potential for carprofen to cause kidney problems, it isn’t common, and I would not have expected this outcome. I too routinely use this medication for my own patients. I understand you are grieving Cloud’s absence, and it is normal to ponder all the “what ifs”. Please know the choices that were made had your dog’s best interest in mind. I hope with time you will be able to allow yourself some grace and let go of the unnecessary burden of guilt. May Cloud’s memory be a blessing in your life. Wishing you the best as you continue life’s journey.
my dog is 13 That diagnosed her with chronic kidney disease giving her fluids she pee everywhere. and drinking water so is there any over counter drugs or new drugs
Hi Brenda,
I am sorry your senior girl has been diagnosed with kidney failure. I am not aware of any new medications that have recently been developed for this condition. I wish I could offer more specific advice, but without playing a personal role in your pup’s medical care it is hard to offer recommendations. I hope you will be able to find the answers you need. Bless you and your sweet girl.
This link has been so helpful. My Joey is a beautiful 14lb Yorkie/Australian terrier mix. I met him when he was 3 days old and knew he was mine. We have been together for 16 years. We recently adopted a little Shipoo (Shit tzu Poodle). She came down with diarrhea and I switched her diet to boiled chicken and rice and she was fine. When Joey experienced diarrhea, I figured it was the same thing and started chicken and rice. Two days later he was no better and threw up three times overnight. He saw our vet the next morning. Blood work showed he was in kidney failure. He gave me the option of bringing Joey to a 24-hour clinic for round the clock IV or putting him on IV in the office. We live in a rural area and the closest 24-hour clinic is at least an hour away. I didn’t want to be so far away from him and opted for the office IV.
I’ve been taking him for 3 days and there was a little improvement and then none. Now he doesn’t want to eat and this is a dog that would devour food. He is lethargic and walks like Bambi. He’s breaking my heart. He was already completely deaf and was losing his site before this happened. He was never a lap dog and now will let me hold him. He’s snoring away next to me as I write this. Doctor assures me he is not in pain. Still he seems very confused.
Waiting to hear back from his doctor now. Yesterday I asked about home euthanasia. I do not want to rush into this but I honestly don’t think he will be getting better. I want to keep him where he feels safe and loved and that is at home. I will be reaching out to a DVM who does hospice and in-home euthanasia. Go figure no 24-hour clinic within miles but there is a hospice doctor in the next town.
Thanks for letting me write this all down and feel a little bit clearer.
Dear Cori,
I am so sorry Joey is starting to decline, and you are facing some difficult decisions about his quality of life. I think it is very wise of you to plan ahead and have an in-home euthanasia doctor ready and waiting for when they are needed. Try to make the most of the time you are gifted and spend each day loving on your sweet boy as much as possible. Wishing you comfort and peace. Bless you both. ♥
My dog will be 5 in May and we found out about his chronic kidney disease about 6 months ago when he had some kind of infection in his neck which was unrelated. All the vets were completely stumped that he could look and act so healthy with creatinine levels between 5 and 6. They did multiple ultrasounds on his kidneys and said they were so unrecognizable they were second guessing they were even his kidneys- obviously they were. He’s like a lab/boxer mix and eats just about anything, runs and walks all the time and has never shown signs of the disease.
Unfortunately this week he got super lethargic and while still eating he stopped drinking water. Today we put him on sub-q liquids at home, Pepcid, and phosphorus binders. He perked up pretty good this afternoon and drank quite a bit of water on his own. We’ll see how it goes with this plan but we know that most dogs are only likely to live 4-6 years so if for any reason he seems like he’s in pain or his quality of life deteriorates we’ll make him comfortable so he can die with dignity.
Dear Val,
I am sorry you are facing this difficult situation with your young dog. I am glad he has been feeling so well until recently and has had a life full of joy and love. I hope the medications and treatments will continue to improve his quality of life and gift you with some extra time together. Thank you for sharing your experience with us. Wishing you continued strength to navigate this tough road ahead. Bless you both.
Our Chihuahua/Terrior mix has Cushings. She has been treated for it and has been doing well. However, while we were visiting with a relative out of town, she got into a hidden bag of Nutramax Dasuquin with MSM Soft Chews for 60-100lb dogs. She began acting lethargic and someone found the empty bag. She then vomited a LOT! There was no poison or overdose information on the bag! I looked online for similar scenarios and most vets advised that a dig might have diarrhea and vomit but that it was a supplement so it should be okay. We called a local vet hospital there and they told us to call Poison Control. She ended up being poisoned from the overdose and was in the hospital for 6 days with kidney failure.. We had to get back home so they gave us bags and needles to do subcutaneous fluids at home. We also have to give her a low fat, low protein diet… basically the opposite diet of what she was on for Cushings. We’ve been doing them for about a week now. We saw the local vet and her BUN levels are really high. They want us to continue with the fluids. She hasn’t had her medication for Cushings for about 2 weeks and that’s really concerning us. She’s losing weigh big time. We tried the prescription diets and she won’t eat them, so we make her a diet of rice, spinach, carrots, broccoli, cauliflower and a small amount of chicken. For treats, we give her dehydrated zucchini and apples. Can you recommend a diet that will help her gain weight that is okay with both kidney disease and Cushings? We are at a loss. We don’t know if we can wean her off the fluids and are concerned that her body will get used to having them so her kidneys won’t function properly. So far, we are $9,000 in for hospitalization, so we want to be sure that she’s comfortable and do all that we can for her. She is a fighter and is doing great! We just need to get some weight on her and don’t know how to do that. I keep forgetting to ask the vet about this and vet appointments are tough to come by locally.
No doubt, we are sending a letter along with all the medical records in a plea to Nutramax to get poison/overdose information on their bag!!!!!
Thank you for any help that you can provide. You article has been a blessing in understanding what is going on with our Nahla!!!
Dear Kelly,
I am so sorry Nahla is fighting these two difficult diagnoses at once. I wish I had some great advice about her diet but with a complicated case like this, I would highly recommend you speak to a specialist. A veterinary nutritionist will be the best source of information for creating a diet that works with Cushing’s and kidney disease. You should be able to find a nutritionist that can prescribe a diet for Nahla based on her specific needs and medical details. I hope your sweet girl can keep fighting and pray she has many happy years ahead. Wishing you all the best of luck. Feel free to leave an update as things progress!
My Rat terrier turn 16 in November2022. It was in August or September I learn she was in Kidney failure. I did not change her diet instead I am treating like a hospice case. Let her eat what she will eat. Giving her kidney meds from her Doctor twice a day. Once she stops eating or drinking then it will be time to say goodbye. Or if she’s in pain. She’s still eating and drinking. Gets around well even blind and deaf. I may get more labs tomorrow to see where her kidneys are now. I do not want to put her down until I know it’s best for her. I think this is the hardest to decide. I see no signs of distress from pain except for today. She was running through the house running into things and when you pick her up she cries and tries to get down. Luckily I had liquid pain killers for her. In about twenty minutes she calm down and has been doing fine since. That’s been hours ago.
Dear Linda,
I am sorry your little pup is nearing the end of her life. I am glad you are able to provide hospice care and keep her at home where she is most comfortable. She is a lucky girl to have spent 16 years making wonderful memories with you. I hope when her time comes, she will pass peacefully. Wishing you strength and courage to face each new day. Bless you both.
. Hi.. i also have a 16 yr old Chihuahua mix with a rat terrier. the vet. suspects early renal disease back in jan. shes on a kidney diet. she likes tbe wet food more than the dry. and take renal supplement twice a day. i was just curious about what pain medication you use? i dont want to use a pain medication thats going to put stress kn her kidneys. she is a ederly dog and does have some joint and arthritis issues
Hi Ally,
I am sorry your senior girl has received this difficult diagnosis. I am glad she will eat the wet food and seems to be doing well with her current treatment regimen. I don’t have a specific pain medication that I use for kidney failure cases. But you are correct you have to avoid certain drugs that can have negative effects on the kidneys. Most vets will probably use some type of opiate or controlled substance to offer very strong pain relief for dogs in end stage kidney failure. If you are looking for safe ways to help with arthritis pain, there are many good options. I will attach links to other articles with more information. Wishing you the best and praying your sweet girl has many happy days ahead.
1. Natural Pain Relief for Dogs: 13 Methods
2. Dog Arthritis Treatment: 8 Ways to Help a Senior Dog at Home
3. How to Relieve Arthritis Pain in Dogs: The Ultimate Guide
Mam, My dog got snake bite on July 15 th nyt…..we didn’t know it was a snake bite….on July 16 th we given him treatment…..that day it self his creatine is 6.6 ……what we have to do !
Hi Vysali,
I am sorry your dog was bit by a snake and now is having issues with his kidneys. Without playing a personal role in his medical care, I can’t offer specific advice or recommendations. Your vet should be able to guide you through this process and let you know what treatment is needed. Hoping for quick answers and a positive outcome for your pup.
Hi Julie, we are currently in the grips of kidney failure with our terrier girl Peach, who is only 4 years old. The vet is stumped as to what caused it but he thinks it could be congenital given her age and that we don’t think she ate anything toxic.
We are on week 5 of IV fluids and a range of different medications. She goes for fluids every 2-3 days. It’s been a rough and intense journey so far going back and forth to the vet and we are drained. She had some really good days where she is bright and wants to eat, then lots of really flat days where we have to spoon food into her. It’s soul destroying and we’re coming to a point where we might have to make a heartbreaking decision… it’s frustrating though because her SDMA test shows she went from a rating of 29 down to 18 which is nearly within normal range. Her BUN is 14 and creatinine is 1.7 so not the worst but still no real improvement in her mood. We aren’t sure what to do next and whether we are fighting a losing battle… any advice so appreciated
Dear Katie,
My heart goes out to you with this difficult and emotional situation you are in with Peach. It sounds like you have a good partnership with your vet and you both are trying everything you can to help restore your pup’s quality of life. Since I haven’t examined your dog myself, it is hard to make specific recommendations. My best advice would be to schedule a consult with an internal medicine specialist. They have a great deal of experience with complicated cases and might know of other testing or treatments to try that can sometimes be cost prohibitive in general practice. I hope you can find some answers that offer a positive outcome for you and your sweet girl. I will attach links to other articles that deal with making tough decisions about when to “let go”. I pray it doesn’t come to this but want you to be prepared just in case. Feel free to leave an update as things progress. Bless you both.
1. Dog Kidney Failure: When to Euthanize Your Dear Dog
2. Using a Quality of Life Scale for Dogs
3. Kidney Disease in Dogs: Stages and What They Mean For Your Dog
My standard poodle Samson was diagnosed with Juvenile Kidney Disease at five months. after his breeder had called to let me know that one of his littermates had died of JKD. Samson is now three years seven months and last week his creatinine and phosphorus levels had dramatically increased. He is in stage three of kidney disease and has begun the subcutaneous hydration treatments and aluminum hydroxide doses in addition to the medication he has been on since diagnosis.
Your article was very helpful even though you don’t discuss JKD . I like your style of writing and clear definitions. I’m curious as to why you did not include or mention the congenital form of kidney disease.
Thank you for your response.
Hi Jill,
I am sorry your sweet boy has struggled with the symptoms of kidney disease his entire life and now it seems to be progressing rather quickly. Juvenile Kidney Disease or congenital kidney dysfunction was not mentioned in the article because this website and the blog articles are all about senior dogs and issues associated with dogs in their senior years. Luckily, most conditions that we write about are applicable for all life stages. I hope the new treatments that have been added to Samson’s daily routine will allow him to have many more happy days ahead. Praying for more time to continue making memories and a good quality of life. Bless you both!
Hi. My 15-pound rescue terrier mix Penny was diagnosed with Stage 3 kidney failure the end of July 2021. I was devastated! SOMA was 21, Creatinine was 4.7 and Bun was 73. She was drinking 32 ounces of water a day. On the recommendation of my vet – I started feeding her Royal Canin renal support (a combo of wet and dry) and giving her Azodyl – (1) in the afternoon and (2) in the middle of the night as she has to wake up every 5 hours to pee. My little bug is still with me over 300 days later although I do see signs of her slowing down. I feel blessed to have this extra time with her.
Hi Dianne,
What a blessing to still be making memories together 300 days later! I am so glad your girl responded to the medications and new diet. Thank you for sharing your experience with our readers as it may help someone else in a similar situation. Praying Penny continues to thrive and is enjoying life. Bless you both!
Maggie is a 8 yr old lab. A 1 1/2 years ago noticed blood in her urine. She was treated with 2 rounds of antibiotics and blood was still present. After MRI she was diag with a tumor on her L kidney. She had surgery to remove the tumor (which was cancerous) and the kidney. She is getting half mature food and half Hills kidney care ( expensive) Due to arthritis she is getting 100 mg vetprofen daily for hips. Also using toe grips to help with slipping on the floor. Her kidney numbers are good. She is active and happy.
Hi Sonia,
I am glad to hear that Maggie is stable and enjoying life! I hope she will continue to thrive and have many happy days ahead. Thank you for sharing your experience with us. Best wishes!
This was informative.
I’ve looked in to kidney disease several times after our girl ate raisins in 2019 that were given to her by a little boy. She was with my husband and he didn’t know they were toxic to dogs. Once he told me (which was hours later), we called the animal poison control, followed their protocol, and then took her to the ER. She received care but was allowed to go home since we weren’t sure exactly how many raisins she’d had (we thought maybe 5 at most). The next day we found 16 raisin in her stool. We took her to her regular vet, where elevated BUN and creatinine levels were determined along with decreased platelets and RDW. Our vet recommended taking her to a 24 hour ER so that she could receive care without having to constantly transport her from our vet’s to the night-only ER and then back again. She got great care including IV fluids, more activated charcoal, and more antiemetics. After about 24 hours we were given the good news that her blood levels had stabilized (at least the BUN and creatinine) – thank you Jesus!
I still closely monitor her blood work. I realize that the “insult” to her kidneys can’t be reversed so I am vigilant about having at least yearly bloodwork.
Hi Amy,
I am happy to hear your girl was able to recover and has been stable for the last few years. You did a wonderful job making sure she received appropriate care quickly after the incident. Routine annual blood work is such a great idea and I wish more dog owners knew how valuable of a tool it can be. Thank you for sharing your experience with us. I hope your sweet pup continues to thrive and I wish you both the best!
My 13 yr old mostly Black Lab stopped eating. Took her to my vet, where her blood work showed elevated kidney numbers…he said he’d seen much worse. He kept her two nights and gave fluids. Her numbers came down some, but are still over the normal range. She was so weak, could not get up from a lying position on her own. I got her to start eating and she is stronger and getting up now., but still a bit weak. She did not have a history of kidney disease before this. Bloodwork a couple years ago was normal.
Hi Janice,
I am glad you were able to get your girl to the vet and treatment started quickly. What a blessing that she is showing improvement and gaining strength! I pray she has a complete recovery and can get back to living her best life. Thank you for sharing your experience with us. Best wishes to you both.
Thank you Dr Julie, once again you have, step by clear step, clarified what we need to understand about our senior Norfolk’s chronic kidney disease diagnosed last summer with bloodwork at her senior exam. It was worrisome after a her pre-dental bloodwork 4 months earlier had been normal. We’d thought her lack of activity was reaction to the recent loss of her lifelong hunting companion, which we all felt deeply. After that diagnosis we immediately started her on low protein diet prepared at home (we’re retired with time for that extra step) and tested her blood monthly for 3-4 months to reassure that she was doing well with the diet. Values didn’t show much change, but she did have an episode of pancreatitis, quickly cleared with meds. We give her sub-q fluids at home, but she can’t appreciate that we’re helping her and we sometimes are tense and she senses that, so we will take her in and vet techs will give the fluids for a small fee when we bring her equipment/fluids with her. The fluids are just extra support right now, she gets 4 small meals a day with equal portion of water on food, and now homemade diet is mixed each meal with equal portion commercial prescription kidney diet. She’s a small gal, so it’s no trouble to mix 3-4 weeks of homemade diet & freeze in small meal size portions. It’s been 6 months since last bloodwork, if this next one is stable I’ll possibly go exclusively to commercial prescription diet. The homemade just gave me the feeling that we were more in control of her care, a necessary illusion when told there’s no magic fix for this, only good maintenance & love.
She naps a lot now, tho her invisible clock is still very accurate about telling us loudly when it’s time to eat, transitioning easily from 2 meals to 4 smaller meals daily, still maintaining her normal healthy 9# weight. She’d like it if we would do out to dig up the yard with her more often as her missing companion would do, but then she sighs & goes back to her nap.
Dear Ani,
Thank you for the kind words and I am glad you found the article helpful. Your little girl is lucky to have such attentive people in her life to advocate for her wellbeing and love her. I pray she continues to do well with the fluids and special diet. I appreciate you taking the time to share your story as it may help someone else in a similar situation. I wish you many more happy days together and fond memories.